


Theme
Student as teacher
INSTITUTION
University College London, Medical School, London

The move to integrated medical school curricula has introduced earlier teaching of clinical skills using Objective Structured Clinical Examinations (OSCEs) for assessment. Compared to written assessments, junior medical students may find the format of the OSCE unfamiliar and intimidating. Senior students are well-placed to provide an introduction to the OSCE.
We devised and delivered a near-peer teaching initiative for first and second year medical students, prior to their first OSCE. This comprised small-group teaching led by students in their penultimate year and focused on developing a confident, structured and professional approach to OSCE stations.
|
Advantages of this approach |
Disadvantages of this approach |
|---|---|
| Senior students are able to draw on past OSCE experiences to highlight practical challenges that the students may face | Senior students lack the clinical experience of faculty members |
| Social and cognitive congruence between junior and senior students facilitates a productive learning environment1 | Basic teaching skills training needs to be provided to the senior students beforehand |
| Fosters a community of mutual educational support |
Many disciplines can be assessed under the remit of the OSCE, making it difficult to design a comprehensive workshop |
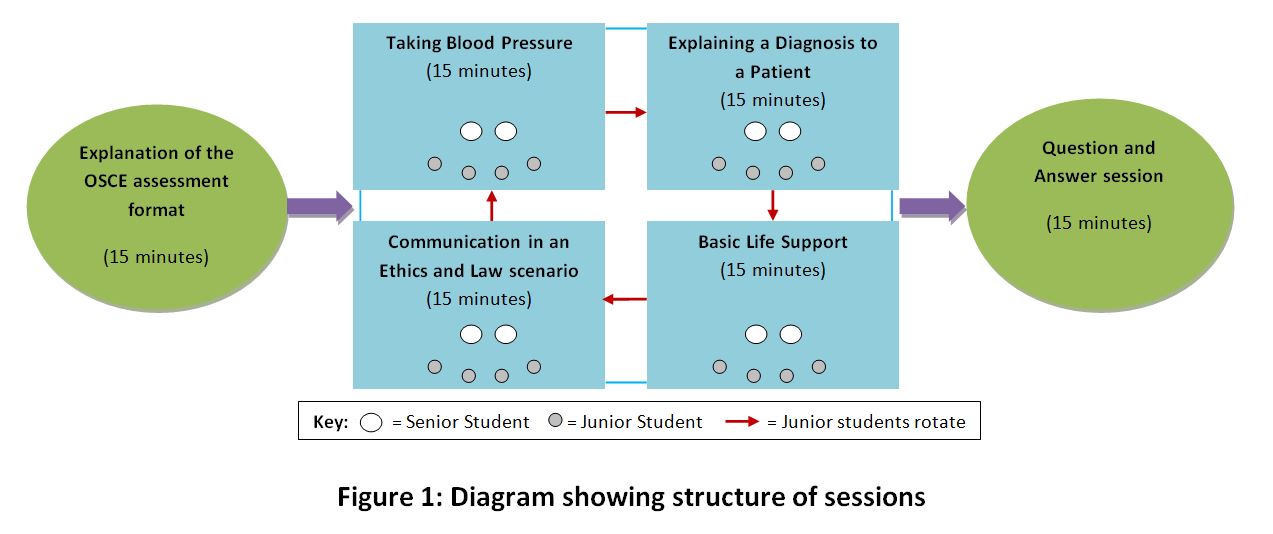
Figure 1 shows the structure of the teaching sessions devised.
Senior students were supplied with example OSCE mark-schemes; however they were instructed to focus on conveying a method to approach the OSCE assessment and to use the specific stations merely as illustrations.
The format was to allow the junior students to tackle the stations in pairs with subsequent feedback and advice from the senior students.
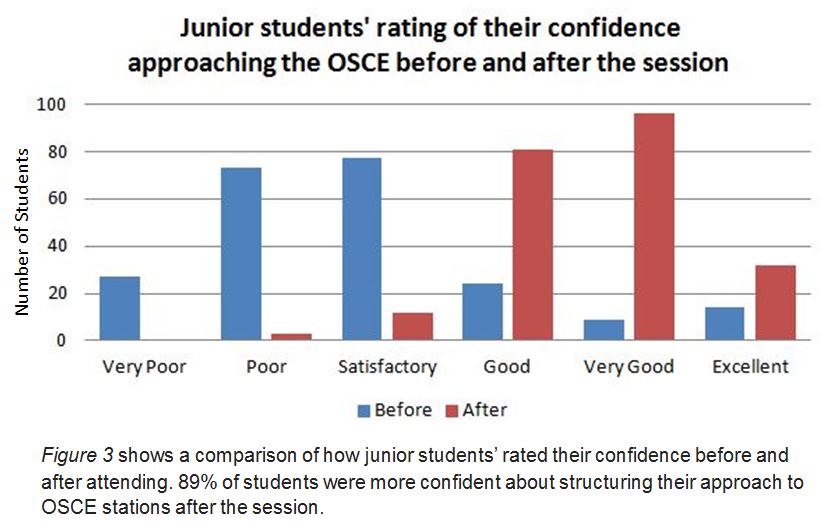
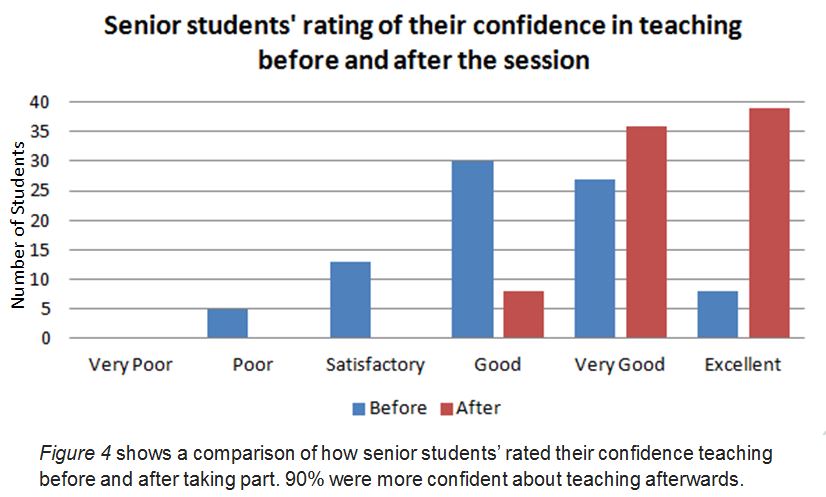
Students attending were asked to complete a feedback form rating a number of parameters on a six-point Likert scale from ‘Very Poor’ to ‘Excellent’. Tutors were asked for their feedback using a similar scale. (See 'more detail' for example feedback forms).
1. Lockspeiser, TM. et al., 2008. Understanding the experience of being taught by peers: the value of social and cognitive congruence. Adv in Health Sci Educ, 13, 361-372.
2. Büscher, R. et al., 2013. Evaluation of the peer teaching program at the University Children’s Hospital Essen- a single center experience. GMS Z Med Ausbild, 30(2), Doc25.
3. Bulte, C. et al., 2007. Student teaching: views of student near-peer teachers and learners. Medical Teacher, 29, 583-590.
Dr Fahad Mahmood, Dr Laura-Jane Smith, Deirdre Wallace, and Professor Jane Dacre for her support.
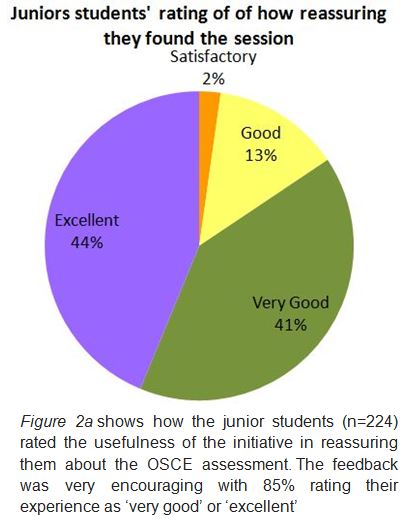
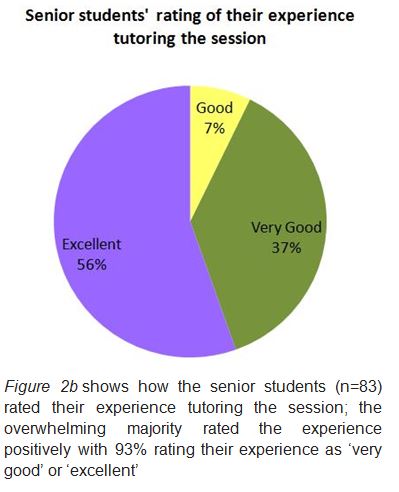
Our teaching initiative successfully reassured and prepared junior students for their OSCE assessment and had additional benefits for the senior students tutoring.
Initiatives using senior medical students to teach practical skills such as basic life support (BLS) are already well established at other medical schools2. These initiatives give senior students an opportunity to develop teaching skills essential for their future career.
They also work towards strengthening a culture of collaborative teaching and learning. Students will be able to continue the cycle of teaching and learning once they have moved up into more senior years and we hope that the framework we have successfully set up will benefit future cohorts of students.
Furthermore, the scope of this approach stands to have impact beyond the mere transfer of knowledge and skills; early interaction of junior students with their senior peers may set good role models3, as well as refocusing those who in the early years can easily lose sight of the goals of medical school.
1. These initiatives are of mutual benefit to both junior and senior students.
2. Senior students are a valuable resource for introducing practical clinical skills and OSCE assessments to junior medical students.
3. Other medical schools can take advantage of this resource-efficient framework to facilitate the introduction of OSCE assessments into integrated curricula.

 Send Email
Send Email