


Theme
Postgraduate Education
INSTITUTION
University of Toronto
Maastricht University
Gordon Center for Research in Medical Education, University of Miami

- Simulation-based mastery learning of Advanced Cardiac Life Support (ACLS) skills is effective
- Traditional ACLS courses incorporate instructor-regulated learning (IRL)
- Directed self-regulated learning (DSRL) may prove to be an effective and less expensive way to teach ACLS skills
- DSRL involves an educator structuring self-regulated learning to ensure appropriate scaffolding exists to optimize learning
Research Questions
- How does the ACLS skill performance of PGY1 Internal Medicine residents who participate in a DSRL simulation-based mastery learning course compare to residents who participate in an instructor regulated learning (IRL) mastery learning course?
- What is the cost effectiveness of a DSRL simulation-based mastery learning course?
Procedure
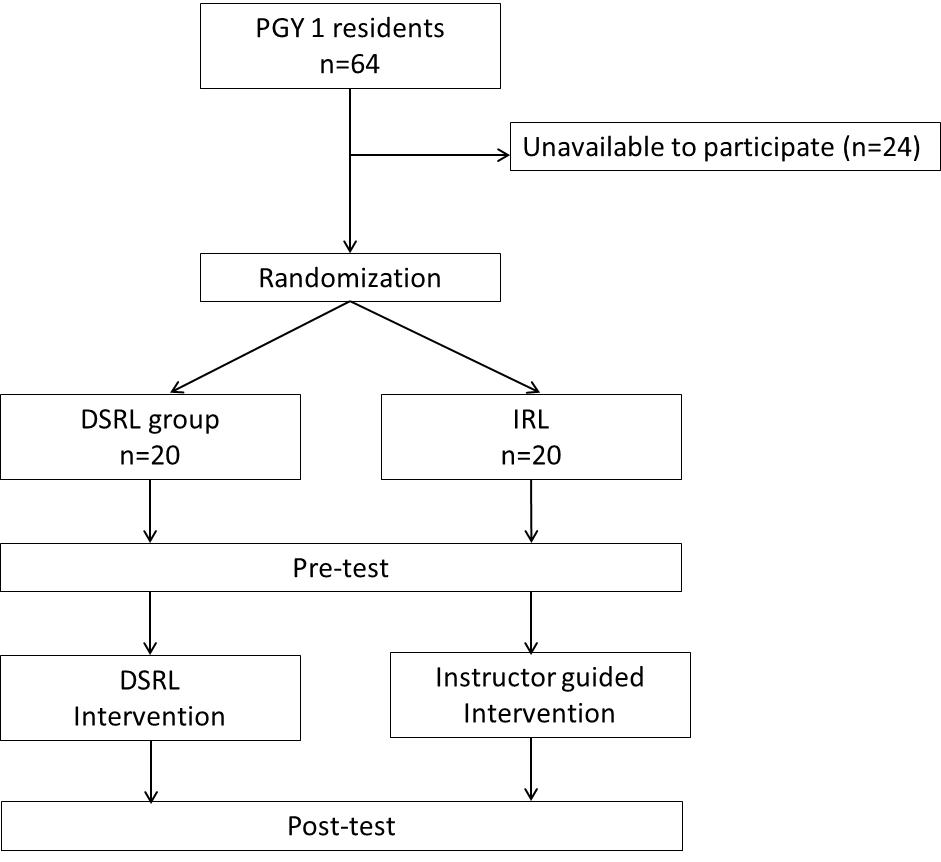
- 40 residents randomly assigned in blocks of four into DSRL or IRL group
- Residents in each group received standard orientation (video - more details), completed a pre-test, received the assessment instruments and minimum passing standard
- Following the intervention, a post-test and post-course survey were completed
Intervention
- Modeled after mastery learning curriculum of Wayne et al. (2006b) and focused on pulseless ACLS events
- Simulation-based training sessions in groups of 4
DSRL Group
- Each group member rotated in role of ACLS team leader for practice scenarios
- After each practice scenario, groups conducted a structured debriefing utilizing a provided debriefing tool
- During the debriefing, residents could review ACLS algorithms, review tips and teaching points developed in advance for each scenario, access any relevant online materials and review the assessment instrument
IRL Group
- Each group received instruction from experienced ACLS instructors
- Scenario selection for testing and practice identical to DSRL group
- Debriefing led by the instructor with access to same debriefing materials as DSRL group
Instruments
- Pre-test and post-test were scored using assessment instruments developed by Wayne et al. (2009), that had been modified based on updated ACLS algorithms
- Pre-tests and post-tests were video-recorded and later scored by a single rater
- 25% of scenarios scored by a second rater
Analysis
- Post-test checklist scores were primary outcome
- Within group differences determined using paired samples t-tests
- Differences between groups determined using ANCOVA, with pre-test scores as covariate
- Intra-class correlation coefficients (ICC) were determined
- ICC = 0.88 - strong inter-rater reliability
- Significant improvement was seen in each group between pre-test and post-test (Table 1)
- Effect size (r) was 0.91 for IRL and 0.95 for DSRL
- No difference between post-test scores in the IRL and DSRL group (controlling for pre-test scores) F(1,37) = 0.007, p = .935
Table 1 - Pre-test and post-test performance. IRL= instructor regulated learning, DSRL - directed self-regulated learning
|
|
IRL= (n=20) | DSRL (n=20) | P value |
| Mean Pre-test score | 71.46 (1.96) | 71.23 (1.31) | .92 |
| Mean Post-test score | 92.97 (1.20) | 93.11 (1.20) | .94 |
- Cost of IRL was higher than DSRL (Table 2)
- Costs of simulation lab rental, equipment, etc. was identical in each group
- Instructor costs were higher in the IRL group, while preparation costs were higher in the DSRL group
Table 2 - Costs associated with each intervention ($Cdn) IRL = instructor regulated learning, DSRL = directed self-regulated learning
| IRL | DSRL | |
| Sim Lab/Simulators | $1200 | $1200 |
| Instructors | $2000 | $0 |
| Technician | $400 | $800 |
| Preparation time | $0 | $1200 |
| Total | $3600 | $3200 |
- DSRL and IRL significantly improve resident performance in responding to pulseless ACLS events, with an average improvement of 22% and with a large effect size (r = 0.9)
- No difference in ACLS skill performance achieved in the DSRL group compared to the IRL group
Costs
- DSRL was more cost effective than IRL for a group of 20 residents
- Although DSRL had higher costs associated with planning and development, savings in instructor costs easily compensated for this
- The cost for 80 residents to complete a DSRL session would be $10400
- The cost for 80 residents to complete an IRL session would be $14400
- Directed Self-Regulated Learning (DSRL) is as effective as Instructor Regulated Learning (IRL) for learning ACLS skills in simulation-based mastery learning
- DSRL is more cost-effective than IRL
This work was completed as part of an MHPE thesis at the University of Maastricht.
This work was supported by a Royal College of Physicians and Surgeons of Canada Fellowship for Studies in Medical Education and through a fellowship provided by the Herbert Ho Ping Kong Centre for Excellence in Education and Practice (CEEP) at the University Health Network, Toronto.
Technical support was provided by Finch Taylor and SimSinai at Mount Sinai Hospital, Toronto.
 Send Email
Send Email