


Theme
Nuclear Medicine
INSTITUTION
Nuclear Medicine Technologist at King Khlaid Hospital- Najran
Kings College London

Pulmonary embolism (PE) is classified as a medical emergency and is caused by blockage of a blood vessel within a deep vein. Due to the serious consequences of pulmonary embolism (PE) and its non-specific symptoms, PE diagnosis is a medical challenge. There is a requirement for accurate diagnostic tools to identify potential patients with PE. This study aims to assess our local experience of combining a low-dose computed tomography (ldCT) with ventilation/perfusion (V/Q) single-photon emission computed tomography (SPECT) for the diagnosis of PE.
Figure (1). Pulmonary embolism physiology. A clot forms in a deep vein, most commonly in the leg, and travels up to the lungs, potentially leading to a blockage within the lungs. The clot can be fatal because it prevents oxygenated blood from reaching vital organs.
The study took the form of a retrospective data collection of patient records for 92 patients with suspected PE between 2017 and 2019 at Guys and St Thomas Hospital at London City. The database study population was derived from the hospital picture archiving communication system. The V/Q-SPECT ldCT has been set at GSTT as a routine diagnosis study for PE for nonpregnant patients. Studies were excluded if the study was of suboptimal quality. A single dual-trained nuclear medicine and radiology consultant performed all reports.
The study consisted of 54 (60%) female patients and 38 (40%) male patients aged 18 to 94 years with a median age of 53 years. In total, 13% of the sample were diagnosed with PE using V/Q SPECT combined with low-dose CT. This finding indicates that V/Q SPECT can result in a higher number of false positives and that CT can be combined to improve the specificity of the technique. 18% would have been reported as positive for PE (5% falsely positive) by VQ SPECT (ie if ldCT not done), If CT had been used as a ventilation substitute, 21% would have been reported as positive for PE (8% falsely positive) by Q SPECT-ldCT.By including ldCT, in cases with no perfusion defect, 8% had incidental findings identified on CT. By including ldCT, in cases with a perfusion defect matched on ventilation, 23% had additional findings.
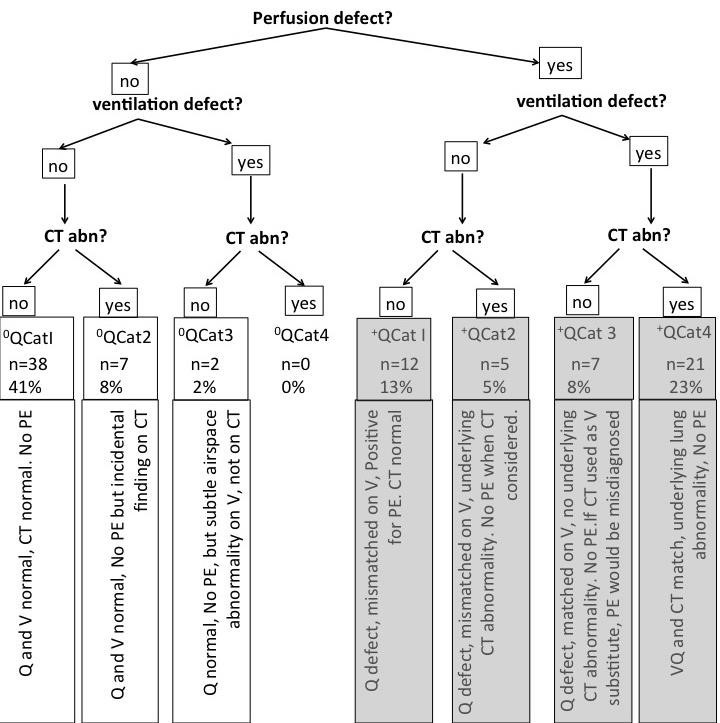
Figure 2. Diagnosis of pulmonary embolism (PE) using ventilation/perfusion (V/Q) single-photon emission computed tomography. (SPECT) with and without additional CT based on a sample size of 92 patients.
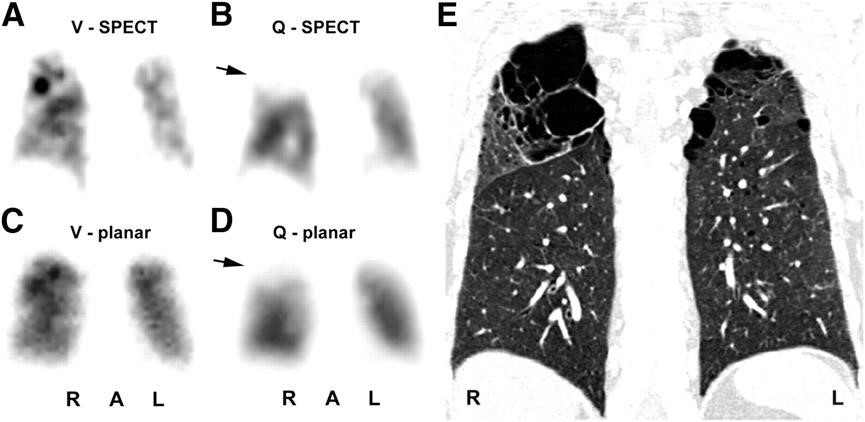
Figure 3. (A–D) Illustration of a false-positive ventilation/perfusion (V/Q) scan as a result of emphysema. The mismatch is most prominent in the right upper lobe. However, computed tomography (CT) scanning (E) indicates the presence of an emphysematous bulla
The current study has demonstrated that there are benefits when combining low-dose CT with the current approaches of V/Q SPECT for the diagnosis of PE. However, the study is associated with a number of limitations, which could be overcome through future work. To improve the degree to which the results of the study could be generalised, a larger scale prospective study based on multi-centres should be carried out. Furthermore, in the current work, a baseline test,such as CTPA, was not used. Such a test could be beneficial in comparing V/Q-SPECT CT with established techniques, such as CTPA. Similar studies have been conducted in the literature but are relatively small scale and are limited by the techniques used. The results of this study were only at the point of interpretation; therefore, the accuracy of the findings has not been assessed.
The study demonstrated that the addition of ldCT to V/Q SPECT increases the specificity of PE diagnosis by identifying pathologies that may otherwise result in a false-positive PE diagnosis for a relatively low-dose of additional radiation. The null hypothesis has been refuted, and we can recommend this strategy.
The secondary aim of the study was to establish whether the ldCT would make an adequate substitute for the ventilation scintigraphic component of the V/Q-SPECT study. Our results demonstrate that if a clear CT scan were to be interpreted as normal ventilation, an additional 8% of patients would have been incorrectly diagnosed as having PE, increasing the false-positive rate. Currently, this approach cannot be recommended.
1- Bajc M. Potential of hybrid V/P SPECT–low-dose CT in lung diagnostics. Breathe. 2012;9(1):48.
2- Le Roux P-Y, Robin P, Delluc A, Abgral R, Palard X, Tissot V, et al. Additional value of combining low-dose computed tomography to V/Q SPECT on a hybrid SPECT-CT camera for pulmonary embolism diagnosis. Nuclear medicine communications. 2015;36(9):922–30.
3- Anderson DR, Kahn SR, Rodger MA, Kovacs MJ, Morris T, Hirsch A, et al. Computed Tomographic Pulmonary Angiography vs Ventilation-Perfusion Lung Scanning in Patients with Suspected Pulmonary EmbolismA Randomized Controlled Trial. JAMA. 2007;298(23):2743–53.
4- Santos J, Carmona S, A. Sequeira J, Prata A, Santos AI. Pulmonary ventilation/perfusion single photon emission tomography – Initial experience of a Nuclear Medicine Department. Revista Portuguesa de Pneumologia (English Edition). 2016;22(1):27– 33.
 Send Email
Send Email