



Theme
Medical Physics
INSTITUTION
Ryerson University, Toronto, Canada
Sunnybrook health sciences center , Toronto, Canada
University of Toronto, Toronto, Canada
- Transrectal Ultrasound (TRUS) has been conventionally used for intraoperative guidance in the high-dose rate brachytherapy (HDR BT) for prostate cancer
- The dominant intraprostatic lesion (DIL) is difficult to visualized using TRUS alone due to image artifacts
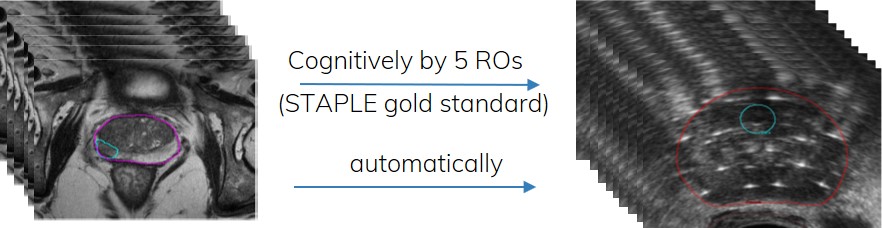
- Incorporation of multi-parametric magnetic resonance (mpMRI) into a TRUS based BT workflow has been proposed to improve the accuracy of DIL delineation
- The geometry of the prostate on mpMRI and on the TRUS may differ significantly, requiring image registration
goal:
To evaluate the efficacy of an in-house, automated image registration software for MRI-to-TRUS DIL fusion (MR2US) and compares its results to two commonly used algorithms: rigid registration, and B-Spline based deformable registration
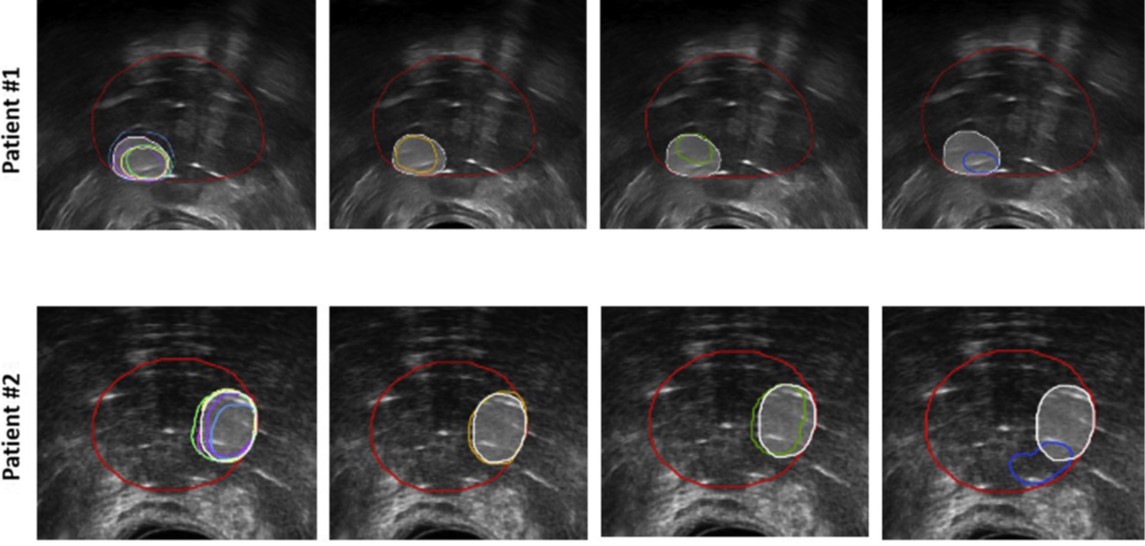
Example of registration results for two patients. (Left to right) Individual ROs’ contours (multiple colors) shown with STAPLE contours (white), MR2US (orange), rigid (green), and B-Spline (blue). The reference TRUS prostate volume is outlined in red. ROs= radiation oncologists; TRUS = transrectal ultrasound; STAPLE = simultaneous truth and performance level estimation
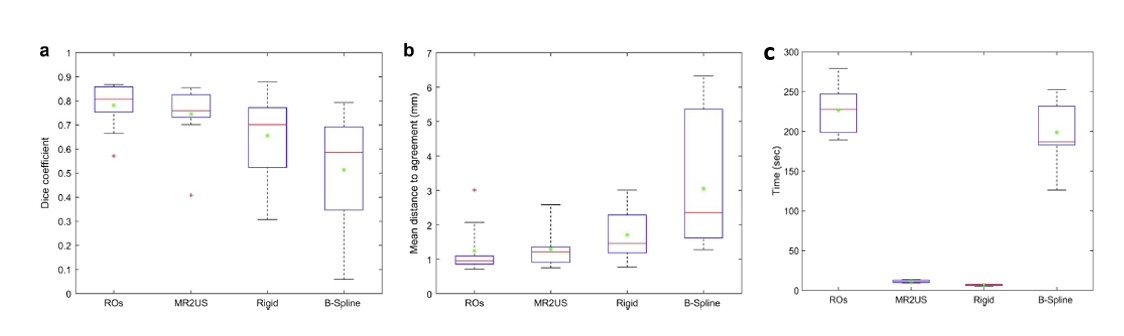
(a) Dice similarity coefficients, (b) mean distance to agreement (MDA) in mm, and (c) Registration time (sec)
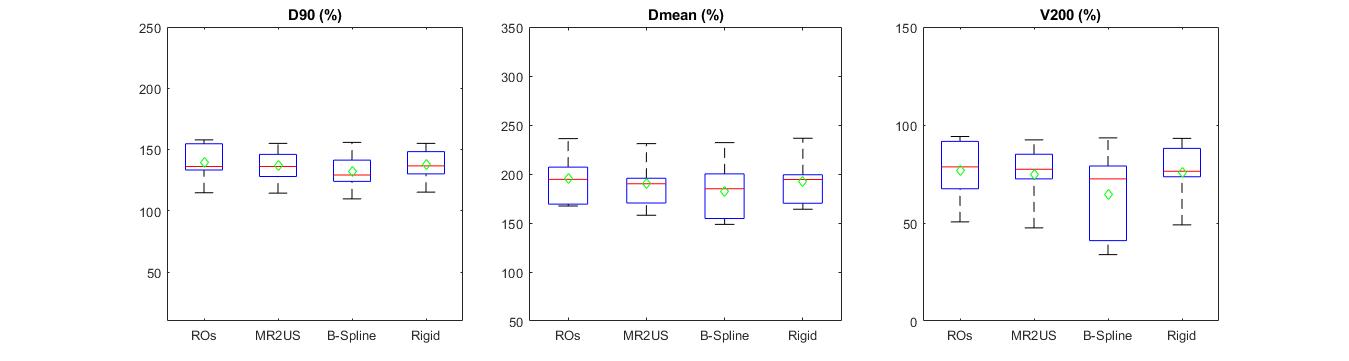
Differences in DIL coverage in terms of D90, Dmean, and V200, respectively
- MR2US registration can reliably register the MRI-defined DIL onto the TRUS image
- Our registration software significantly improved the registration compared to the rigid and B-spline methods
- MR2US accounts for prostate deformation induced by the TRUS probe
- No statistical differences were observed between rigid and MR2US registration algorithms in terms of DIL coverage
- B-Spline should not be used for MR-to-TRUS registration for DIL-targeted prostate brachytherapy
The authors gratefully acknowledge The Ministry of Higher Education of Saudi Arabia (King Faisal Specialist Hospital & Research Center, Riyadh) and the Prostate Cancer Fight Foundation for funding
- A. Shaaer, M. Davidson, et al., "Clinical evaluation of an MRI-to-ultrasound deformable image registration algorithm for prostate brachytherapy", Brachytherapy., vol.18,pp. 95-102 , 2018
- O. Ukimura, A. Marien, et al., “Trans-rectal ultrasound visibility of prostate lesions identified by magnetic resonance imaging increases accuracy of image-fusion targeted biopsies,” World J. Urol., vol. 33, no. 11, pp. 1669–1676, 2015
- S.K. Warfield, K.H. Zou, and W.M. Wells, “Simultaneous truth and performance level estimation (STAPLE),” IEEE Trans Med Imaging, vol. 23, no. 7, pp. 903–921, 2004.
- “Plastimatch.” [Online]. Available: http://www.plastimatch.org/.
- “3D Slicer v.4.8.”
- K.K. Brock, S. Mutic, et al., “Use of image registration and fusion algorithms and techniques in radiotherapy: Report of the AAPM Radiation Therapy Committee Task Group No. 132: Report,” Med. Phys., vol. 44, no. 7, pp. e43–e76, 2017.
 Send Email
Send Email