



Theme
Medical Physics
INSTITUTION
Ryerson University, Toronto, Canada
Sunnybrook health sciences center, Toronto, Canada
University of Toronto, Toronto, Canada
- Prostate brachytherapy procedure is operator experience dependent that requires training to ensure high quality outcomes
- There is presently inadequate training opportunities for the TRUS-based brachytherapy procedure during radiation oncology residency programs
- The use of prostate brachytherapy has continued to decline, which results in a substantial reduction in training opportunities
Goal:
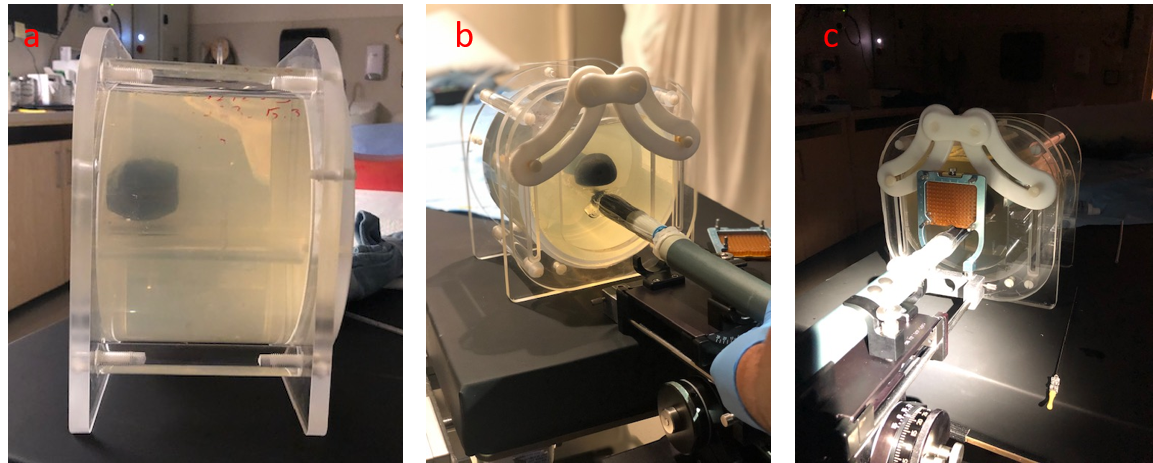
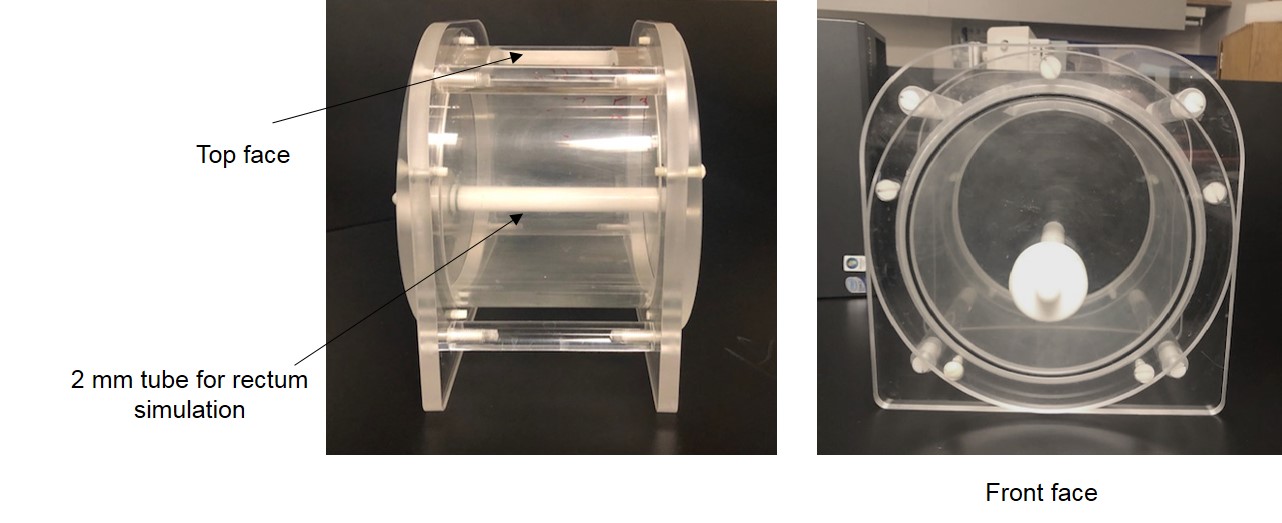
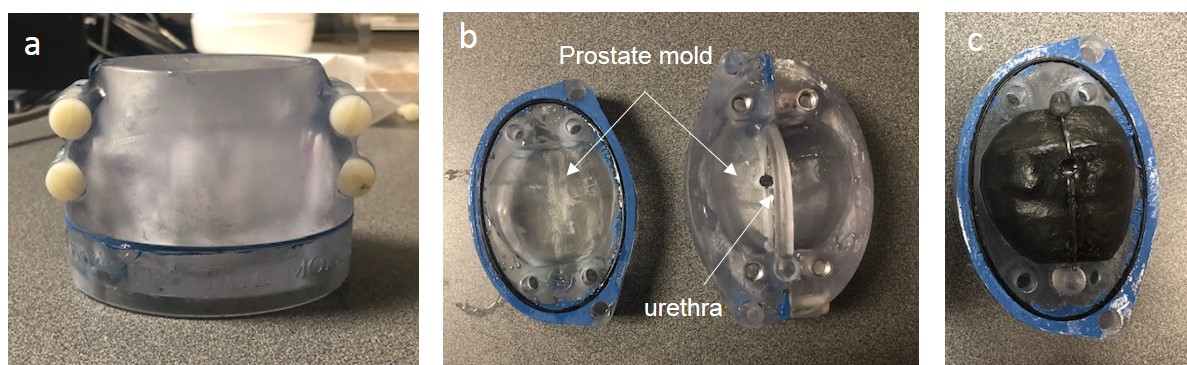
To develop an in-house gelatin-based prostate phantom for training purposes during ultrasound-based prostate brachytherapy procedures
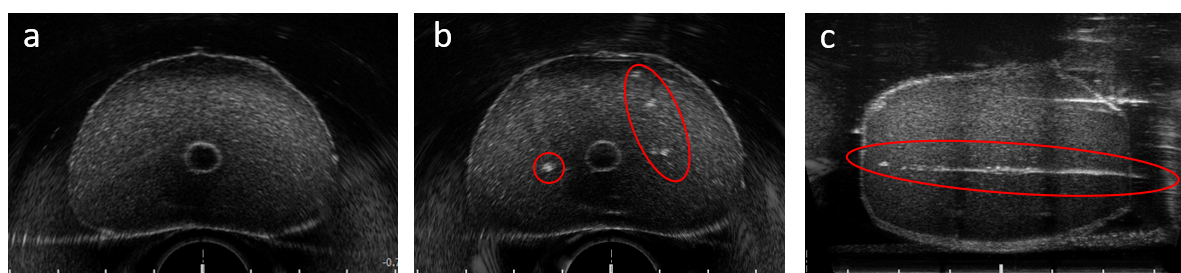
Ultrasound images of the phantom before and after needles insertion
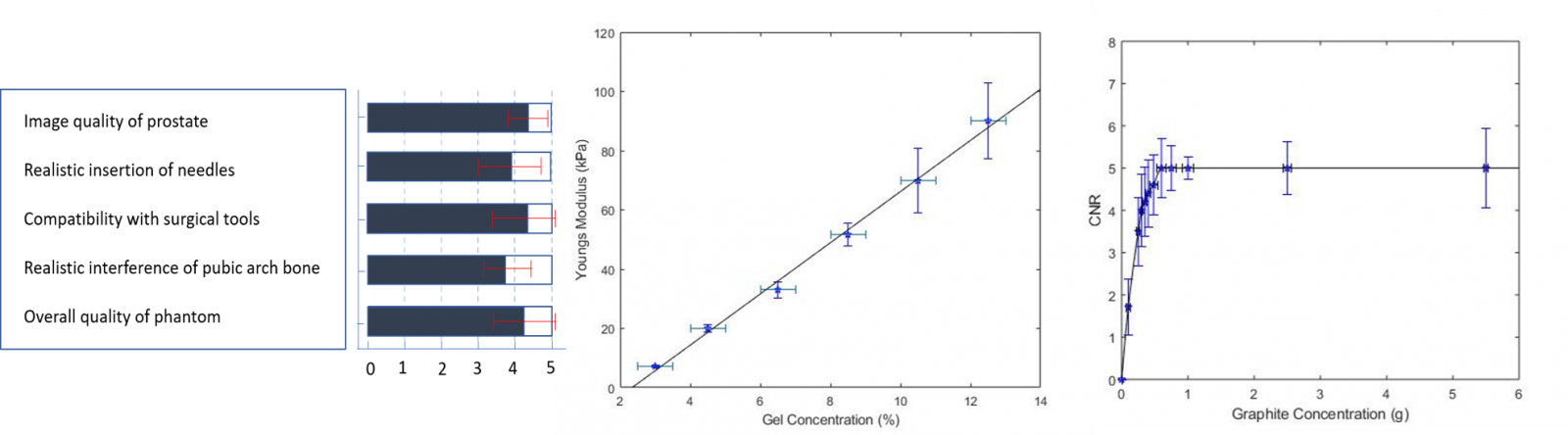
Left to right: Survey results, Young's modulus vs. gelatin concentration, and CNR as a function of scattering agent concentration, respectively
- We have developed a 3D printing prostate phantom to be used for training purposes during interstitial prostate brachytherapy
- Based on the results, the reconstructed phantom could be used as an anthropomorphic surrogates for ultrasound imaging during brachytherapy procedures
The authors gratefully acknowledge the help of Ross Williams at Sunnybrook Research Insititute for his assisstance with the US elastography measurements. The authors also would like to thank The Ministry of Higher Education of Saudi Arabia (King Faisal Specialist Hospital & Research Center, Riyadh) and the Prostate Cancer Fight Foundation for funding
- M. Gaudet, J. Jaswal, and M. Keyes, “Current state of brachytherapy teaching in Canada: A national survey ofradiation oncologists, residents, and fellows,” Brachytherapy, vol. 14, no. 2, pp. 197–201, 2015.
- “Summary of ACGME Program requirements for graduate medical education in radiation oncology changes. Effective July 1, 2020.,” no. 1, pp. 1–4.
- P.F. Orio, P.L. Nguyen, et al., “Prostate Brachytherapy Case Volumes by Academic and Nonacademic Practices: Implications for Future Residency Training,” Int. J. Radiat. Oncol. Biol. Phys., vol. 96, no. 3, pp. 624–628, 2016.
- W.R. Lee, “Brachytherapy Experience in Radiation Oncology Residency Programs in the United States-From Bad to Worse,” Brachytherapy, vol. 15, no. 2016, p. S174, 2016.
 Send Email
Send Email