
 |
Title
Spectrum of Magnetic Resonance Cholangiopancreatography Findings in Acute Cholecystitis

Theme
Diagnostic & Interventional Radiology
Background
To highlight spectrum of findings on Magnetic Resonance Cholangiopancreatography (MRCP) in patients with acute cholecystitis. To determine length of hospital stay in operated cases.
Summary of Work
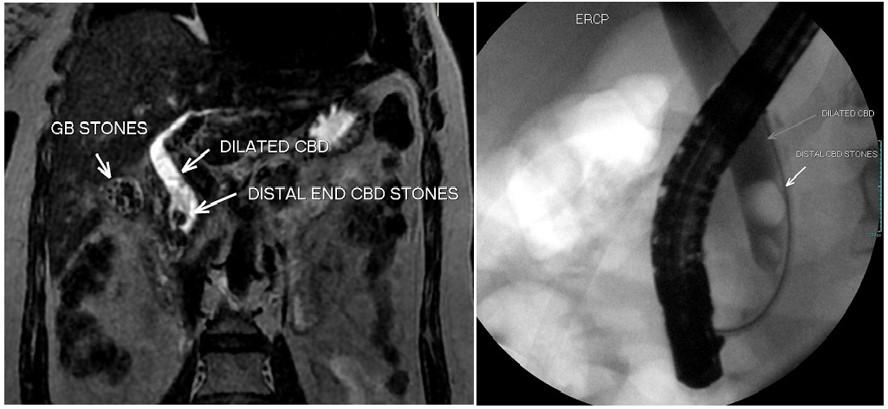
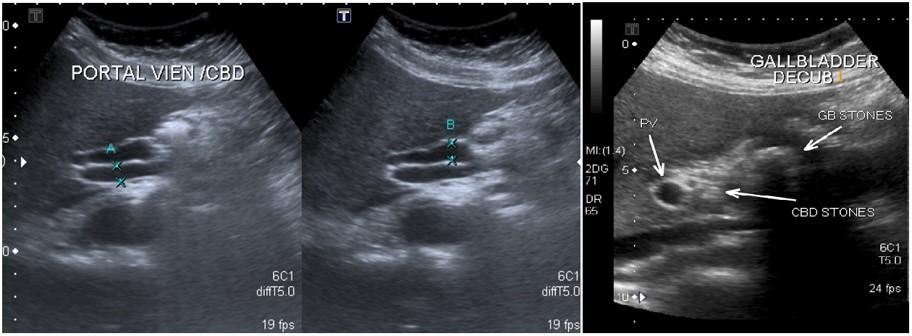
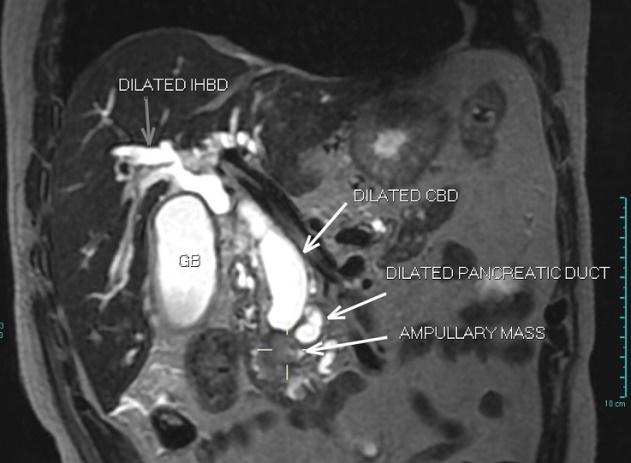
This retrospective observational study was conducted in Radiology department at our hospital in Dhahran, from August 2016-2018. All patients who presented with acute cholecystitis, obstructive liver pattern or deranged liver tests, and underwent MRCP (on a 1.5 Tesla scanner) were evaluated. Patients with chronic cholecystitis, previous hepatobiliary surgery, pregnant patients and those contraindicated to MRI were excluded. Patterns of MRCP findings were categorized as: (i) acute cholecystitis with normal CBD, (ii) acute cholecystitis with dilated CBD and cause identifiable, (iii) acute cholecystitis with dilated CBD and cause not identifiable. Any associated biliary ductal variants or anomalies (e.g., pancreas divisum, choledochal cyst, low insertion of CBD) were also documented. Operated cases were followed to determine length of hospital stay after open or laparoscopic procedures. Chi-square and t-test were used to determine association.
Summary of Results
Of the 104 patients, majority (60%) were females. The mean age was 43 years. Two-thirds of patients were having normal CBDs (68.3%), while nearly one-third (31.7%) had dilated CBDs, and half of these (16.4%) showed an identifiable cause of obstruction. Thirteen patients (12.5%) had associated anomalies. The length of hospital stay was seen significantly less in laparoscopic than with open cholecystectomies (p=.0005).
Conclusion
Magnetic resonance cholangiopancreatography is helpful to identify causes and anomalies in patients with acute cholecystitis patients having deranged or obstructive liver function.
Take-home Messages
Magnetic resonance cholangiopancreatography is helpful to improved efficiency service for patients presenting as acute surgical admissions also detect any associated biliary ductal variants or anomalies. Patient selection is crucial, as this will lead to further interventions that could potentially be cost beneficial.
References
1. Halpin, V. (2014). Acute cholecystitis. BMJ clinical evidence, 2014.
2. Bagla, P., Sarria, J. C., & Riall, T. S. (2016). Management of acute cholecystitis. Current opinion in infectious diseases, 29(5), 508-513.
3. Nasr, M. M. (2017). An innovative emergency laparoscopic cholecystectomy technique; early results towards complication free surgery. Journal of Gastrointestinal Surgery, 21(2), 302-311.
4. Khan, S. U., Soh, J. Y., Muhibullah, N., Peleki, A., Abdullah, M., & Waterland, P. W. (2019). Emergency Laparoscopic Cholecystectomy: Is Dedicated Hot Gall Bladder List Cost Effective?. Journal of Ayub Medical College Abbottabad, 31(1), 3-7.
5. Costi, R., Gnocchi, A., Di Mario, F., & Sarli, L. (2014). Diagnosis and management of choledocholithiasis in the golden age of imaging, endoscopy and laparoscopy. World Journal of Gastroenterology: WJG, 20(37), 13382.
6. Oppenheimer, D. C., & Rubens, D. J. (2019). Sonography of Acute Cholecystitis and Its Mimics. Radiologic Clinics, 57(3), 535-548.
7. Qiu, Y., Yang, Z., Li, Z., Zhang, W., & Xue, D. (2015). Is preoperative MRCP necessary for patients with gallstones? An analysis of the factors related to missed diagnosis of choledocholithiasis by preoperative ultrasound. BMC gastroenterology, 15(1), 158.
8. Petrescu, I., Bratu, A. M., Petrescu, S., Popa, B. V., Cristian, D., & Burcos, T. (2015). CT vs. MRCP in choledocholithiasis jaundice. Journal of medicine and life, 8(2), 226.
9. Wong, H. P., Chiu, Y. L., Shiu, B. H., & Ho, L. C. (2012). Preoperative MRCP to detect choledocholithiasis in acute calculous cholecystitis. Journal of Hepato Biliary Pancreatic Sciences, 19(4), 458-464.
10. Singh, A., Mann, H. S., Thukral, C. L., & Singh, N. R. (2014). Diagnostic accuracy of MRCP as compared to ultrasound/CT in patients with obstructive jaundice. Journal of clinical and diagnostic research: JCDR, 8(3), 103.
11. Bates, D. D., LeBedis, C. A., Soto, J. A., & Gupta, A. (2016). Use of magnetic resonance in pancreaticobiliary emergencies. Magnetic Resonance Imaging Clinics, 24(2), 433-448.
12. Chang, J. H., Lee, I. S., Lim, Y. S., Jung, S. H., Paik, C. N., Kim, H. K., & Jung, I. S. (2012). Role of magnetic resonance cholangiopancreatography for choledocholithiasis: analysis of patients with negative MRCP. Scandinavian journal of gastroenterology, 47(2), 217-224.
13. Tonolini, M., Ravelli, A., Villa, C., & Bianco, R. (2012). Urgent MRI with MR cholangiopancreatography (MRCP) of acute cholecystitis and related complications: diagnostic role and spectrum of imaging findings. Emergency radiology, 19(4), 341-348.
14. Chen, J. E., Kadribegic, A., & Sarkany, D. (2019). Bilirubin Correlation May Preclude MRCP in Acute Cholecystitis Patients With Normal Common Bile Duct Diameter. American Journal of Roentgenology, 212(5), 1018-1023.
15. Chisholm, P. R., Patel, A. H., Law, R. J., Schulman, A. R., Bedi, A. O., Kwon, R. S., ... & Prabhu, A. (2019). Preoperative predictors of choledocholithiasis in patients presenting with acute calculous cholecystitis. Gastrointestinal endoscopy, 89(5), 977-983.
16. Boys, J. A., Doorly, M. G., Zehetner, J., Dhanireddy, K. K., & Senagore, A. J. (2014). Can ultrasound common bile duct diameter predict common bile duct stones in the setting of acute cholecystitis?. The American Journal of Surgery, 207(3), 432-435.
17. Al-Jiffry, B. O., Elfateh, A., Chundrigar, T., Othman, B., AlMalki, O., Rayza, F., ... & Hatem, M. (2013). Non-invasive assessment of choledocholithiasis in patients with gallstones and abnormal liver function. World Journal of Gastroenterology: WJG, 19(35), 5877.
18. Sinha, R., Gardner, T., Padala, K., Greenaway, J. R., & Joy, D. (2015). Double-Duct Sign in the Clinical Context. Pancreas, 44(6), 967-970.
19. Barut, B., Gönültaş, F., Gök, A. F. K., & Şahin, T. T. (2019). Management of Acute Cholecystitis During Pregnancy: A Single Center Experience. Ulusal travma ve acil cerrahi dergisi= Turkish journal of trauma & emergency surgery: TJTES, 25(2), 154-158.
20. Kang, S. K., Heacock, L., Doshi, A. M., Ream, J. R., Sun, J., & Babb, J. S. (2017). Comparative performance of non-contrast MRI with HASTE vs. contrast-enhanced MRI/3D-MRCP for possible choledocholithiasis in hospitalized patients. Abdominal Radiology, 42(6), 1650-1658.
21. Tonolini, M., Ierardi, A. M., Patella, F., & Carrafiello, G. (2018). Early cross-sectional imaging following open and laparoscopic cholecystectomy: a primer for radiologists. Insights into imaging, 9(6), 925-941.
22. Loozen, C. S., Oor, J. E., van Ramshorst, B., van Santvoort, H. C., & Boerma, D. (2017). Conservative treatment of acute cholecystitis: a systematic review and pooled analysis. Surgical endoscopy, 31(2), 504-515.
