| ePOSTER | ||
| Theme: Best Practice in Teaching and Learning |

|
| Abstract Title |
 |
|
| Students' perception towards medical simulation training as a method for clinical teaching | ||

|
Authors: |
Marwa A. El Naggar1 Abdulrahman H. Almaeen2 |
Institutions: | 1 Assistant Professor in Medical Education, Faculty of Medicine, Jouf University, Kingdom of Saudi 1 Lecturer, Medical Education Department, Faculty of Medicine, Suez Canal University, Egypt 2 Assistant Professor, Department of Pathology, Vice Dean, Faculty of Medicine, Jouf University. |


The Faculty of Medicine, Jouf University (FOM-JU) adopted innovative integrated educational strategies like Problem-Based Learning (PBL), Team-Based Learning (TBL), Community Oriented Education (COE), Simulation-Based Learning (SBL), Student-centered seminars, interactive lectures, and early hands-on training in a safe learning environment, i.e. in clinical skills labs
Mastery of clinical skills (CS) is central to the transformation of a medical undergraduate student into a competent health professional fit for medical practice
Unfortunately, deterioration of the clinical skills level of medical graduates has recently been noted which could be due to difficulty in training on the patients due to humane, religious, or social reasons or allotment of less time for training. For the previous reasons, developing clinical skills units in medical schools has become mandatory in the study of medicine 1
2 Simulation-based learning can help mitigate this tension by developing health professionals’ knowledge, skills, and attitudes while protecting patients from unnecessary risk





Numerous reports support the introduction of simulation-based medical education as an important step in curriculum development 3
Learning skills on a simulator is less stressful for both the trainee and the teacher, and helps increase the trainee's self-confidence. Major advantages of learning skills on a simulator are: each procedure can be interrupted, improved and repeated until the required proficiency has been achieved, and no real harm is done when an eventual mistake – inadmissible in real clinical setting – is made on a mannequin 4
College of medicine at Jouf University has four longitudinal courses, designated as clinical skills lab 1, 2, 3 and 4. The main aim of these courses is to familiarize our students, in the preclinical phase, with a diverse number of necessary clinical skills before embarking on the clinical phase where they should be exposed to real patients in hospitals and clinical units. The program extends longitudinally throughout the curriculum from year 1 to year 3 and is coordinated with the block/system and the learning problems
Every Clinical skills lab topic is integrated with the topic of educational problem; e.g. training of our students undertaking the cardiovascular block on how to examine the heart; starting with inspection followed by palpation, percussion and then auscultation utilizing Harvey®: the Cardiopulmonary Patient Simulator,
Rational: SBL is implemented in our college involving all students in different study years (i.e. from year 1 to year 5) for which a necessity for measuring their perception towards such a learning strategy is emerging. However, Saudi medical students’ perception towards SBL was measured but at a low scale
Aim: This study was aimed to explore the perception of medical undergraduate students towards SBL as a method for clinical teaching. A total of 410 male and female students, in preclinical and clinical phases, were surveyed.
Methodology
A cross-sectional study was conducted at the Faculty of medicine, Jouf University (FOM- JU), Sakaka, KSA, 2018. From its inception, FOM- JU adopted simulation-based learning as one of numerous educational strategies. First-three-year medical students learn clinical skills under the supervision of specialized instructors who give introductory lecture addressing the skill of interest, then students will be divided into small groups (i.e. 7 -10 students in each) with an assigned tutor who supervises them during hands-on training and eventually assesses them.
In the present study, the sample encompassed all students of FOMJU of both genders who are exposed to SBL (i.e. the 1st-, 2nd-, 3rd-, 4th- and 5th-year male students whereas female students span all years except the fifth since the most advanced batch of them falls in the 4th-year level upon conducting the study)
Valid and reliable questionnaire developed by Agha et al (2015) 5 was used, with minor modifications of some of the questions. Questionnaire is a 5-point Likert scale assesses the overall students’ satisfaction, and challenges students faced during simulation learning. The percentage of satisfaction of all students was calculated by combining frequency of levels of satisfaction (satisfied and very satisfied) for each item in the questionnaire. The responses on the Likert scale were totaled for each domain (from 1=very dissatisfied to 5=very satisfied). Survey was distributed electronically to all students by batch emails, on blackboard and via whatsApp
Statistical Analysis
Survey responses were summarized using frequency and percentage. The percentage of satisfaction of all students was calculated by combining frequency of levels of satisfaction (satisfied and very satisfied) for each item in the questionnaire. Difference between satisfied and unsatisfied students in preclinical and clinical phases were calculated using chi square test. Inferential statistics using independent samples t-test was used to compare the difference between the satisfaction and challenges scores by the phase of study and the gender. P < 0.05 was considered statistically significa
A questionnaire was distributed to all medical students (total number: 410 students; 277 males & 133 females), the response rate was 56% (n= 230). 32.6% (n=75), 29.7% (n=68), 23.8% (n=55), 1.8% (n=4) and 12.2% (n=28) from the 1st, 2nd, 3rd , 4th and 5th years, respectively
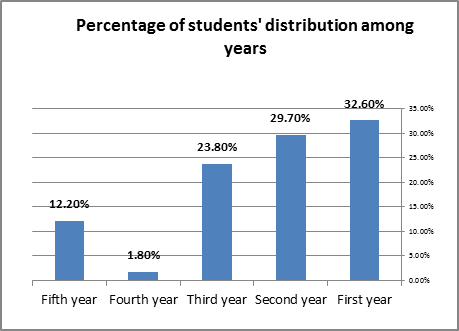
Figure 2: Percentage of students' distribution among year
86%n=198) were from the preclinical phase (i.e. the 1st, 2nd and 3rd years) whereas 14% (n=32) were from the clinical phase (i.e. the 4th and 5th years). The age of 53.4% (n=123) of participants ranged from 20-23 years old. Most of the students (69%) assured that the introductory lectures are clear and comprehensive, 77.6% found their information updated, 81% said that the intended learning outcomes of the lectures are mentioned in the start, 74% agreed that the instructors describe the indications, contraindications, risks, common complications and the process of the procedure and they believed that each session promotes active participation and subgroup hands-on training promotes deeper understanding of the skill figure 3
Figure3: Percentage of medical students' satisfaction with clinical skills lab 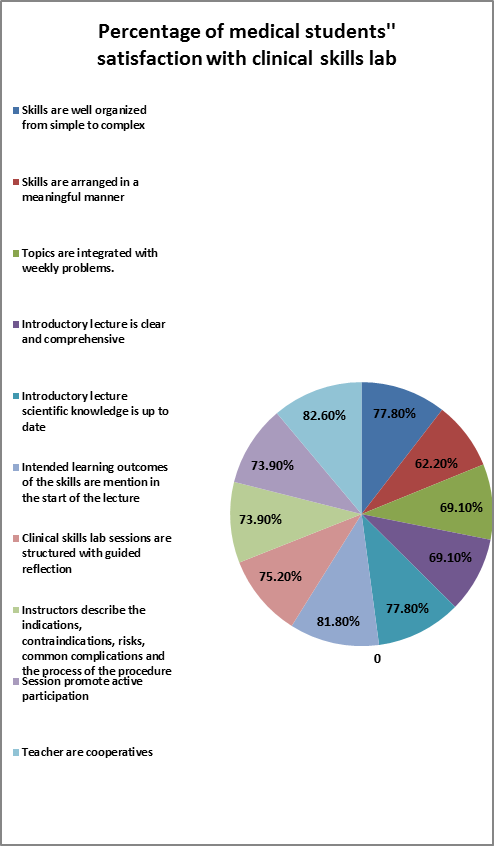
(Table 1: Percentage of students' satisfaction with simulated based learning (n=230
|
Percentage |
Students' satisfaction with simulated based learning |
|
81.0 |
Patient simulators are a useful addition to learning with real patients |
|
80.0 |
I would like more training with simulators |
|
80.0 |
I am familiar with the concept of simulation based learning |
|
77.40 |
Simulation based learning is a useful learning strategy |
|
81.0 |
Simulation based learning made the subject more interesting |
|
77.0 |
Simulation based learning helped me to apply what I learnt |
|
79.80 |
Simulation based learning should be included in the courses frequently |
|
82.50 |
Simulation based learning helped me retain knowledge |
|
83.0 |
Simulation based learning provided a semi-realistic experience |
|
76.0 |
Simulation based learning helped me in communication skills |
|
72.20 |
I felt comfortable with the simulated environment |
|
81.70 |
Simulation based learning developed clinical decision making |
|
86.0 |
Cooperation between the students is important for practicing at the skills-laboratory |
|
77.50 |
Assessment of clinical skills lab is fair |
|
79.0 |
Assessment of clinical skills lab is matching with the way I being trained |
Furthermore, the majority of students (80%) found that patient simulators are a useful addition to learning on real patients, they are familiar with the concept SBL, they need more training on simulators, 82% reported that simulation-based learning has developed their clinical decision making, 86% stated that cooperation between the students is important for practicing at the skills laboratory (table 1). With regards to challenges, 22.6%, 17.4% and 34.5% of participants reported that models are enough, training labs are suitable for training and the time allocated for skills lab is appropriate, respectively. 81% reported thatinstructor gave them the opportunity to practice at the skills laboratory
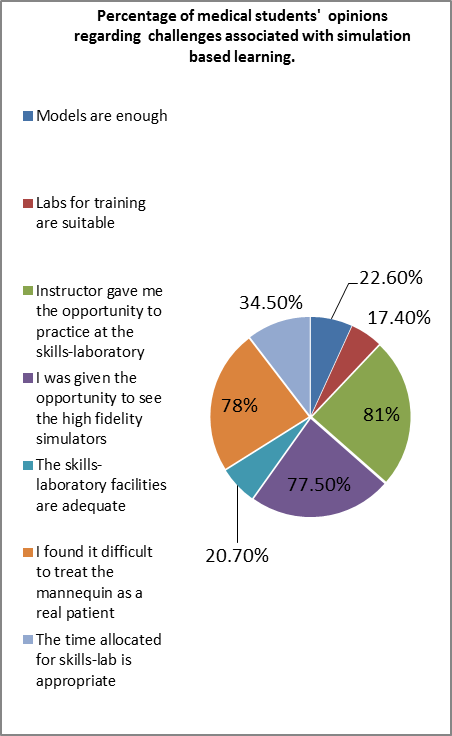
Figure 5: Percentage of medical students' opinions regarding challenges associated with simulation based learning n=230
Table 4. Comparison of satisfaction and challenges with simulated-based learning by the phase of 230 medical students.
|
Phase with score |
N |
Mean ±SD |
P-value |
|
Total score satisfaction 0.001 |
|||
|
Preclinical phase |
198 |
63 ± 9 |
|
|
Clinical phase |
32 |
52±7 |
|
|
Total score challenges |
|||
|
Preclinical phase |
198 |
18±5.2 |
0.20 |
|
Clinical phase |
32 |
19±.6.3 |
|
|
Total score |
|||
|
Preclinical phase |
198 |
81±2 |
0.04* |
|
Clinical phase |
32 |
72±3 |
|
P < .05 was considered statistically significant.

Study limitations
Limited response rate of the clinical-phase students
Study evaluated the first level only of Kirkpatrick’s four-level model
Perception of faculty members towards SBL was not measure
Recommendation 
Provision of more simulators and mannequins in order to better match the number of students
Hastening up the process of moving to the new college-of-medicine building which is located in the main campus, more modernized and spacious
Introduction of more advanced high fidelity models and simulated three-dimensional computer models as more computer-assisted learning packages become available for students' training
Introduction of VPs, computer-based cases, and virtual cadavers ; that will be programmed to dynamically adapt to provide feedback and meet learner-specific needs
Conclusion 
The study concluded that use of simulation laboratory is of great benefit to the students and a great teaching tool for the staff to ensure students learn various skills, also the majoritey of FOM-JU students were satisfied that SBL improved their clinical skills, retentionof learning material; enhance clinical decision making and communicating with patients
Medical educators must be open to new strategies available in the vast simulation toolbox to best meet their students' diverse learning needs
The authors would like to thank FOMJU Clinical skills lab co-coordinators
- Goodfellow P, and Claydon P, Students sitting medical finals—ready to be house officers? Journal of royal society of medicine, 2001.
- Hundert E and Epstien R, defining and assessing professional competences, Journal of American medical association, 2002.
- Vesna P and Matej C, the value of clinical simulation –based learning, medicone, 2007.
- Fatimah L, Simulation-based learning: Just like the real thing, J Emerg Trauma Shock. 2010.
- Agha A, Asma Y, Alhamrani, Muhammad A., Satisfaction of medical students with simulation based learning, Saudi Med J 2015.
 Send Email
Send Email