
| Theme: 7BB Approaches to teaching and learning | |||
 |
||||||
| A study to explore student opinion on the changing electrocardiographic terminology and its effect on the teaching |
 |
|||||
|
||||||
The replacement of the term posterior ischemia/infarction to describe the reciprocal electrocardiographic changes in leads V1, V2, V3 by the term lateral was suggested, because magnetic resonance imaging have demonstrated the oblique position of the heart within the thorax and so the region referred to as the posterior wall (based on anatomic and pathological studies of ex vivo hearts) was lateral rather than posterior (1, 2, 3). We explored student opinion on this change and its effect on the teaching.
The third year students of medicine of the Lithuanian University of Health Sciences (two groups, n = 10 and n = 8), and the second year students of this university (one group, n = 10) – total 28 students of medicine answered the questions which terminology - posterior or lateral they prefer, and why. Previously they had the short explanation of the history of this terminology and underwent the teaching in two ways – using the term posterior and lateral. Electrocardiography was explained using two diagrams: 1 - the hex axial reference system based on the six limb leads of the 12 lead electrocardiogram - to view the heart's electrical activity in the frontal plane (Fig. 1), 2 - the hex axial reference system based on the six chest leads - to view the heart's electrical activity in the horizontal plane (Fig. 2).
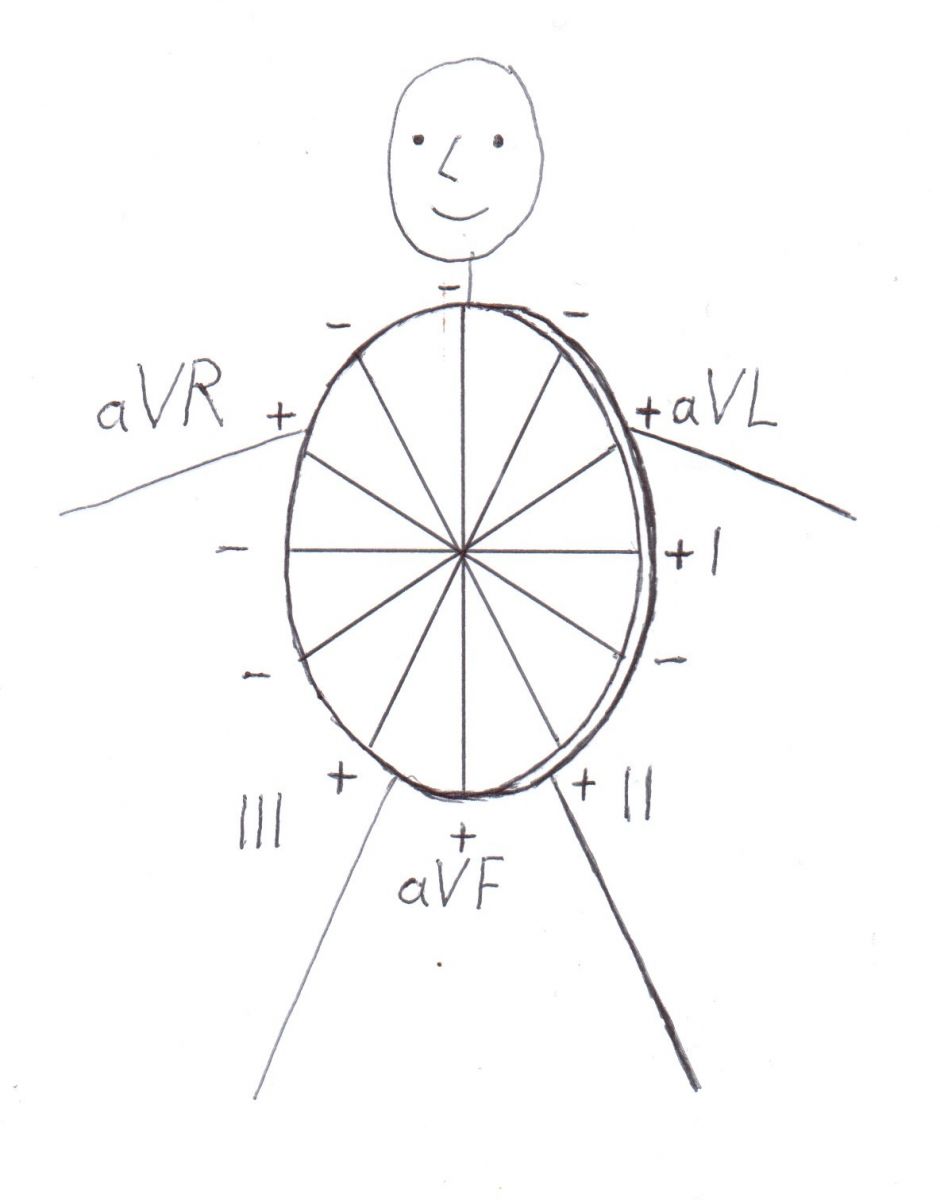
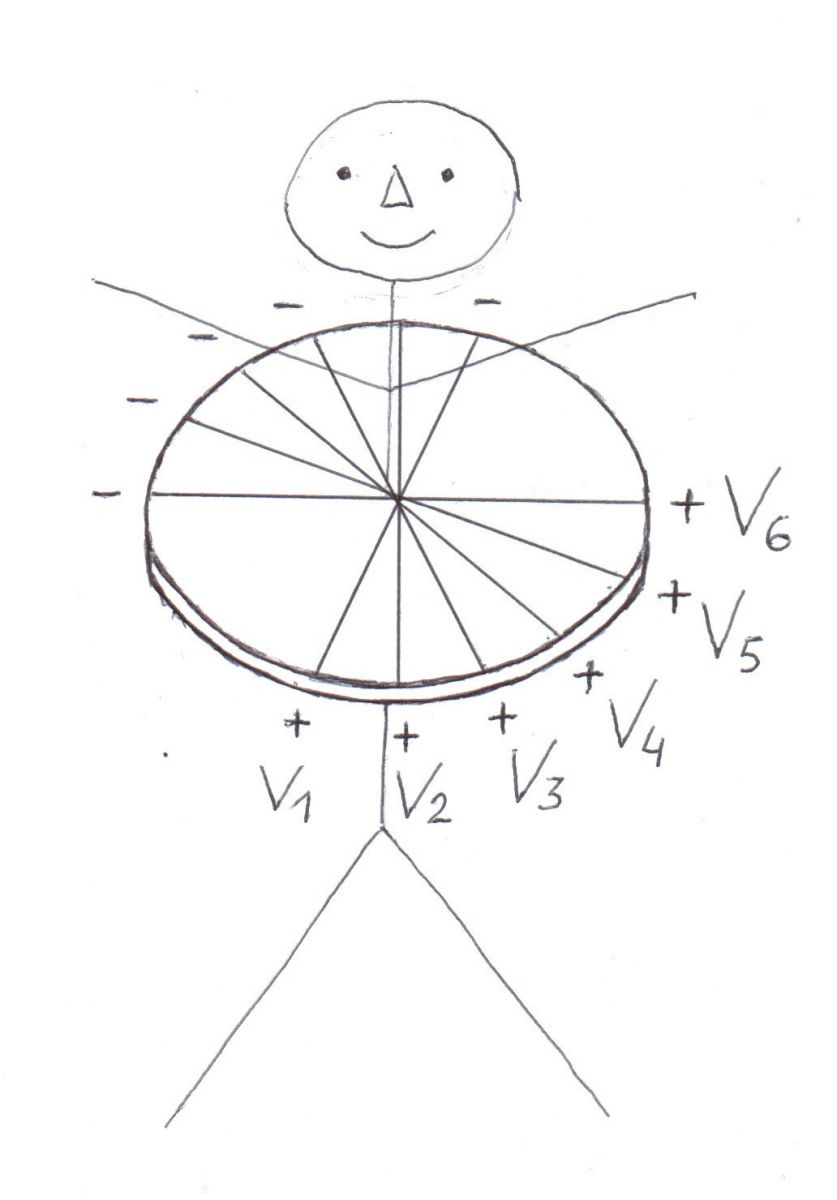
Fig. 1 (left). The hex axial reference system based on six limb leads to view the heart's electrical activity in the frontal plane.
Fig. 2 (right). The hex axial reference system based on six chest leads to view the heart's electrical activity in the horizontal plane.
Extending the chest leads onto the back (Fig. 3) and adding leads V7, V8 and V9 to the diagram based on the six chest leads (Fig. 4) the reciprocal changes in leads V1, V2, V3 were explained.
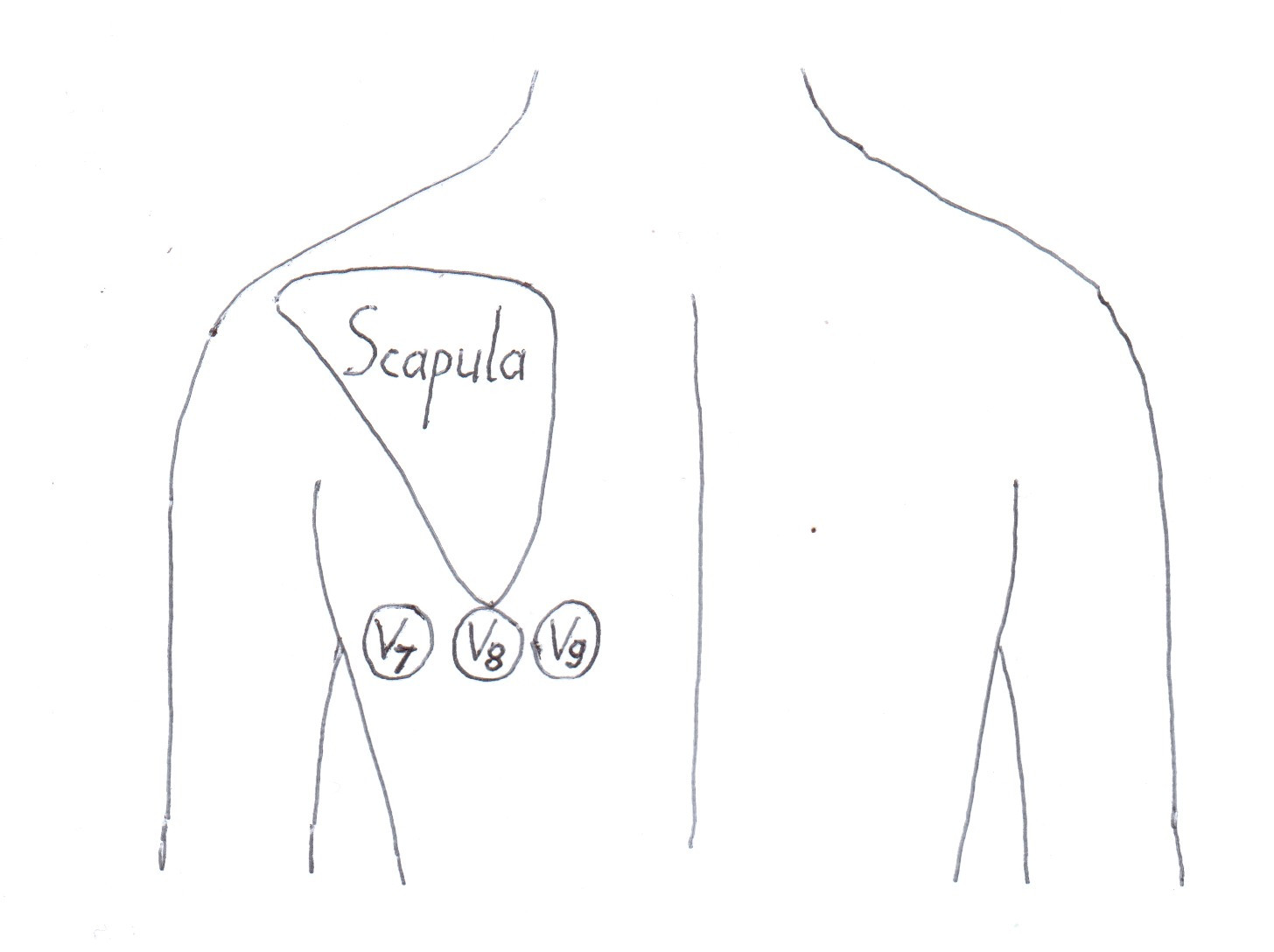
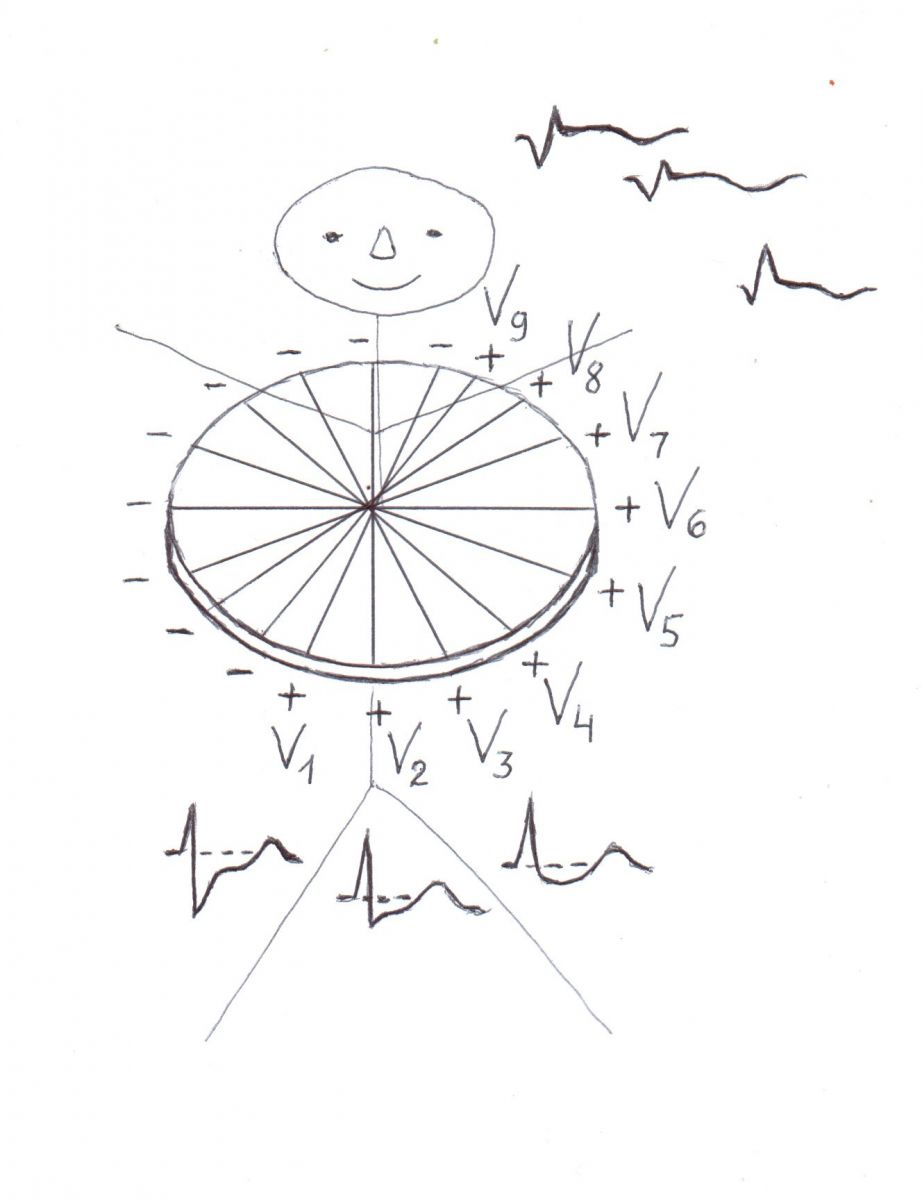
Fig. 3. Recording of the additional leads V7, V8 and V9 extended onto the back.
Fig. 4. The diagram with the additional chest leads V7, V8 and V9 to explain the reciprocal changes in leads V1, V2, V3.
All students preferred the term posterior: all the second year students - as more understandable explanation of electrocardiography and the third year students in both groups - mainly due to various complications that may arise from this change (Fig. 5). Another part of the third year students answered that they prefer the term posterior as more understandable explanation of electrocardiography.
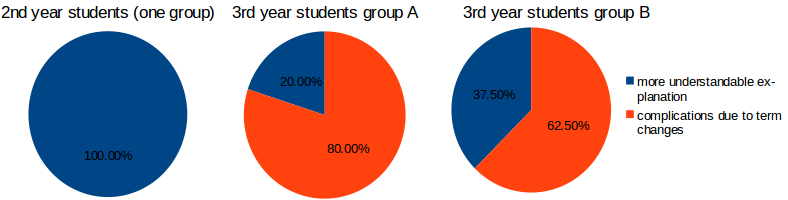
Fig. 5. Student opinion on the changing electrocardiographic terminology: causes of the preferred term posterior.
Our study showed that students prefer the term posterior as more understandable explanation of electrocardiography and due to various complications that may arise from the changing electrocardiographic terminology. Because the term anterior was unchanged, the term posterior should be used to describe ischemia/infarction in the opposite location.
Teaching should be simple and understandable.
-
Gorgels APM, Van der Weg K. Posterior or lateral involvement in nonanterior wall infarction. What's in a name? J Electrocardiol 2010;43:221.
-
Bayés de Luna A, Wagner G, Birnbaum Y, et al. A new terminology for the left ventricular walls and for the location of myocardial infarcts that present Q wave based on the standard of cardiac magnetic resonance imaging. A statement for healthcare professionals from a committee appointed by the International Society for Holter and Non Invasive Electrocardiography. Circulation 2006;114:1755.
-
Bayes de Luna A, Cino J, Goldwasser D, et al. New electrocardiographic diagnostic criteria for the pathologic R waves in leads V1 and V2 of anatomically lateral myocardial infarction. J Electrocardiol 2008;41:413.

 Send Email
Send Email