


Theme
eP2 ePosters 2
INSTITUTION
Barts and The London School of Medicine and Dentistry - Institute of Health Science Education - London - United Kingdom

The use of Virtual Patients (VPs) in medical education is a long-established learning tool within e-learning. Considerable time and resources may be invested into creating VPs. The independent utilisation of these VPs can however be low by undergraduate students when the resource is not used directly as part of the curriculum. We designed and created a VP utilising elements of personalisation and tailored feedback and integrated its delivery into a small group tutorial. We aimed to assess whether VP’s used in the context of a tutorial increase clinical knowledge and the ability to apply it.
A Linear branching VP was constructed using Articulate Storyline for an undergraduate paediatric curriculum. The VP utilised referenced word variables to add personalisation of names of students (Image 1); referenced number variables were used to determine tailored feedback, assign illustrated characters to students and to add points to students scores whilst completing interactive quizzes. The VP also contained a mixture of short answer, extended matching and single best answer questions. These questions were not part of the pre or post quiz used in our evaluations. Prior to being used by students the VP was peer reviewed by senior paediatricians.
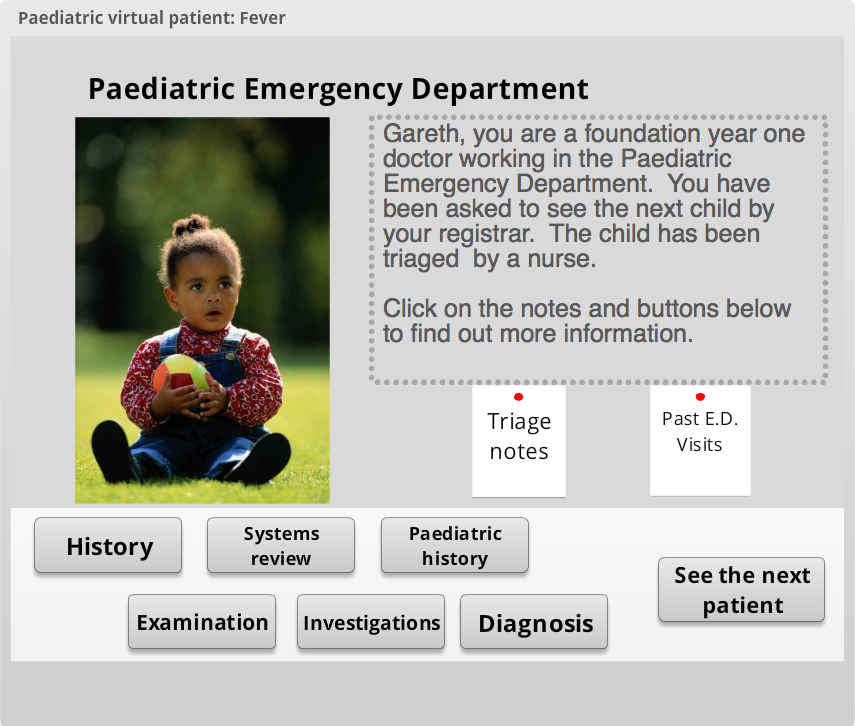
Image 1. Initial home screen showing personalised name using word variable for the student "Gareth"
34 students completed the same VP prior to their fourth year clinical attachment in paediatrics in a tutorial setting with an E-learning clinical fellow. Prior to and after completing the VP-case 21 students were assessed on their ability to identify appropriate history items (as a % correct from 5 items). They were also evaluated on their ability to identify appropriate physical examination and clinical guidelines from a scenario (correct/incorrect). All students completed a satisfaction questionnaire of the VP tutorial. Students were not provided with any additional speciality specific information prior to testing other than use of the VP.
There was a high degree of satisfaction in the paediatric virtual patient tutorial with students enjoying the tutorial (82%) and feeling actively engaged in the VP consultation (85%). Importantly, most students found the case challenging (82%) and reflective of clinical practice, with clinical reasoning skills also being utilised (88%). A smaller number of students thought that the VP alone would be useful for their future learning (76%).
| Before | After | Statistical- Significance | |
| Percentage of history items correctly identified - Mean (SD) | 56% (SD 14%) | 98% (SD 6%) | Paired t=9.1; p<0.001 |
| Correct physical examination identified (%) | 54% | 100% | Fishers exact p=0.015 |
| Correct guideline identified (%) | 8% | 85% | Fishers exact p=<0.001 |
Table 1. Pre and post-test scores of knowledge following virtual patient tutorial.
There was a significant increase in knowledge of paediatric guidelines (p=<0.001) and interpretation of a clinical scenario to select the correct examination (p= 0.015) following completion of the virtual patient (Table 1.). Knowledge of the paediatric history also increased significantly in pre and post virtual patient testing (p<0.001).
The use of a blended learning approach coupling tutorials with VPs encouraged students to engage in the use of VPs. It had high levels of satisfaction amongst the students, and the VP in this context also increased knowledge and challenged reasoning skills.
1. VP tutorials represent a suitable method of utilising VPs
2. Students enjoyed the tutorials
3. In a small cohort the tutorials increased knowledge in paediatrics
Further studies will aim to address the retention of knowledge gained.
 Send Email
Send Email