


Theme
8II Mobile learning
INSTITUTION
Chang Gung University of Science and Technology - Nursing
Tao-yuan, Taiwan
Increasing the awareness of health literacy and the impact of limited health literacy among all healthcare providers would be a worthwhile endeavor. Low health literacy (LHL) is recognized as a serious public health problem due to its widespread prevalence and significant impact on patient outcomes. Health professionals must take an active role in identifying and assisting such patients. Furthermore, medical education needs to include health literacy training in curricula.
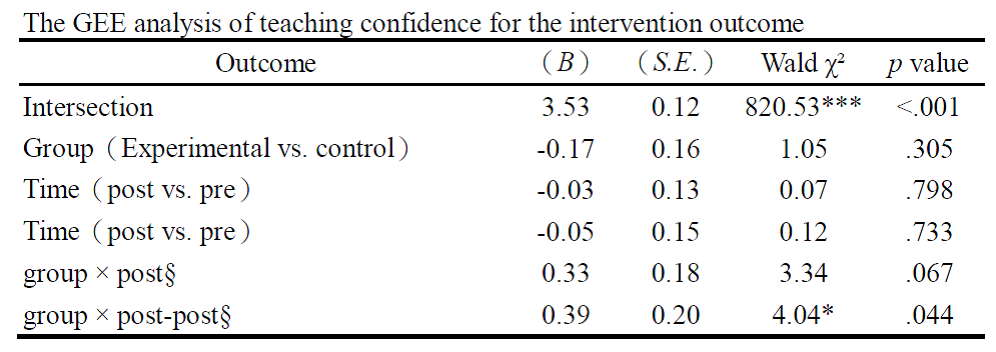
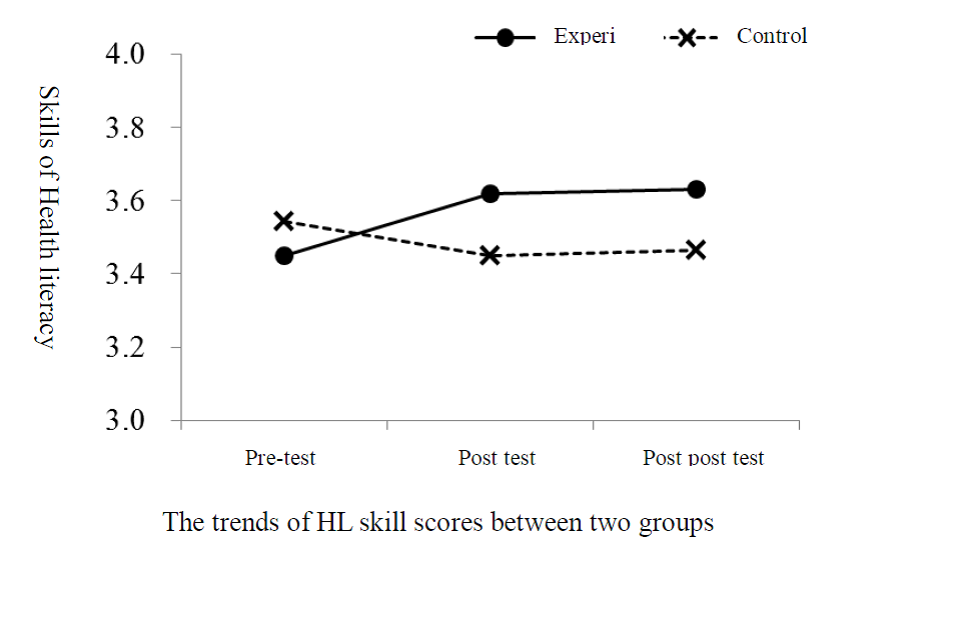
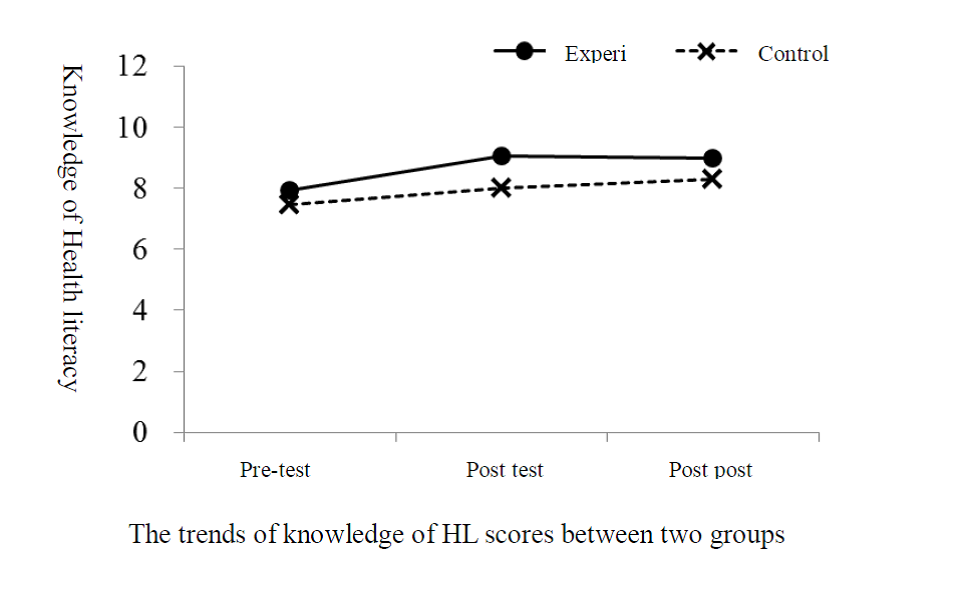
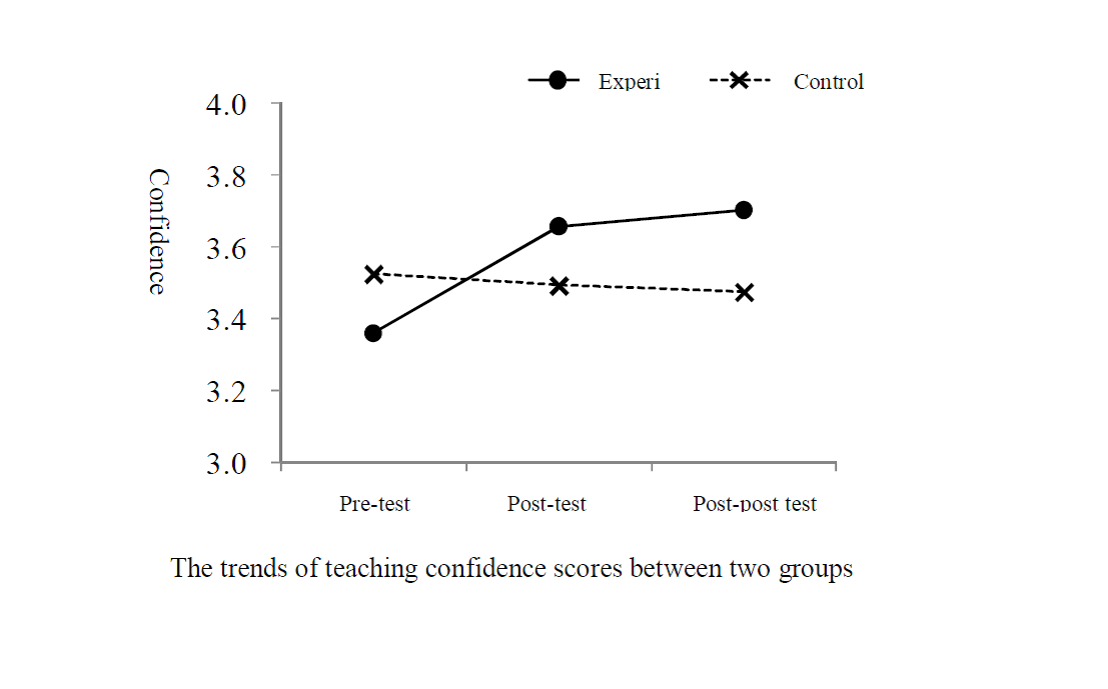
The results of the study showed that medical professionals have 60-70% understanding towards health literacy, and the use of related strategies was found to be around 70%. Analysis of the results of each item indicated that the uses of important health literacy strategies are still hindered by difficulties and limitations. Though the results of this study demonstrated that these online programs managed to introduce improvements to the understanding of health literacy concepts and characteristics as well as the educational techniques, strategies, and effectiveness of low health literacy, these changes did not reach statistical significance. Only experimental group exhibited a greater degree of improvement in the confidence in the education of low health literacy during the post-posttest than did the control group, and provided evidence of the effectiveness of the online simulation curriculum.
At the end of the 3-month online course, a total of 168 participants remained, with 88 participant forming the experimental group and 80 forming the control group. Although the improvements of the understanding of LHL characteristics, the educational techniques, strategies, and effectiveness of low health literacy, these changes did not reach statistical significance. Only experimental group exhibited improvement in the confidence in the LHL education during the post-posttest than did the control group.
.png)
Though supported by hospitals, there is still room for discussion in terms of the program’s degree of participation and feedback. Also, it was discovered that 3 participants have yet to access the program and only completed the Q&A. Whether this will affect the effectiveness of the intervention awaits further investigation as more diversified platforms with more features will be created for increasing participation.
Conrick, M., Dunne, A., & Skinner, J. (1995). Learning together: using simulation to foster the integration of theory and practice. The Australian Electronic Journal of Nursing Education, 1(1), 2-9.
Eggenberger, S. K., & Regan, M. (2010). Expanding simulation to teach family nursing. Journal of nursing Education, 49(10), 550-558.
Institute of Medicine (2004). Health literacy: A prescription to end confusion. Washington, DC: Author.
Kameg, K., Clochesy, J., Mitchell, A. M., & Suresky, J. M.(2010).The Impact of high fidelity human simulation on self-efficacy of communication skills. Issues in Mental Health Nursing, 31,315-323.
Kripalani, S., Jacobson, K., Brown, S., Manning, K., Rask, K. J., & Jacobson, T. A. (2006). Development and implementation of a health literacy training program for medical residents. Medical Education Online, 11(13), 1-8.
McLellan, H. (1996). Situated learning: Multiple perspectives. In H. McLellan (Ed.), Situated learning perspectives (pp5-17). Englewood Cliffs, NJ: Educational Technology.
Price-Haywood, E. G., Roth, K., Shelby, K., Cooper, L. A. (2009). Cancer risk communication with low health literacy patients: A continuing medical education program. Journal of General Internal Medicine, 25(S2), 126-129.
Roter Ironside, P. M., Jeffries, P. R., & Martin, A. (2009). Fostering patient safety competencies using multiple-patient simulation experiences. Nursing Outlook, 57(6), 332-337.
Schillinger, D., Pitette, J., Grumbach, K., et al. (2003). Closing the loop: physician communication with diabetic patients who have low health literacy. Archieve Internal Medicine, 163, 83-90.
Schlichting, J. A., Quinn, M.T., Heuer, L. J., Schaefer, C.T., Drum, M. L., & Chin, M. H. (2007). Provider perceptions of limited health literacy in community health centers. Patient Education and Counseling, 69 , 114-120.
Zavertnik, J. E., Huff, T. A., & Munro, C. L. (2010).Innovative approach to teaching communication skills to nursing students. Journal of Nursing Education, 49(2),65-71.
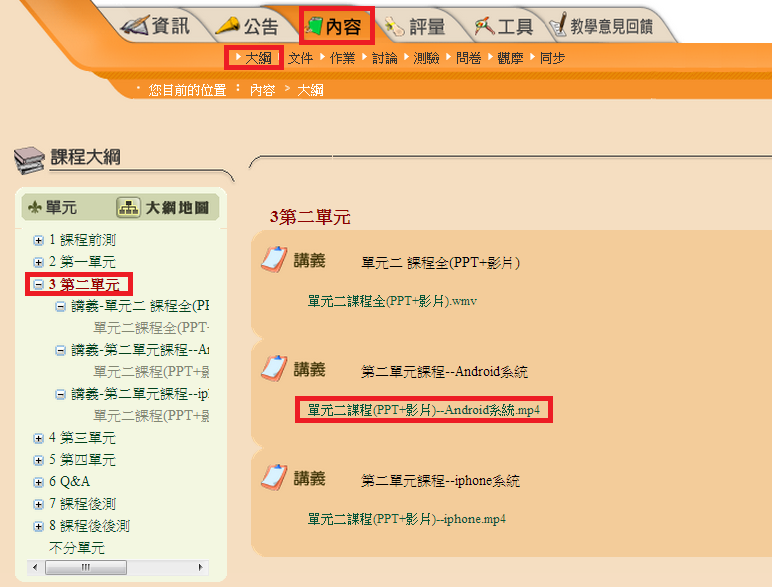
The online simulation curriculum contained four chapters with four patients with LHL that health professionals may encounter in their clinical settings. Four competences must be established including the ability to identify the characteristics of low health literacy, to understand the tools for assessing health literacy, to show confidence in the education of individuals with low health literacy and to use educational strategies for patients with LHL. Online lecture, scenario-based videos, active feedback and online examination are adopted and integrated the 16-hours curriculum. After curriculum development, we transform the curriculum package into Android, iphone and PC versions for participants using in various smart devices.
This study adopted a quasi-experimental design with nonequivalent pretest and posttest for one medical center and several hospitals in northern Taiwan. Four competences of the online simulation curriculum include the ability to identify the LHL characteristics, to understand the tools for assessing health literacy, to show confidence in the education of individuals with LHL and to use educational strategies for patients with LHL. Online lecture, scenario-based videos, active feedback and online examination are adopted and integrated into the 16-hours curriculum. After curriculum development, we transform the curriculum package into Android, iphone and PC versions for participants using in various smart devices.
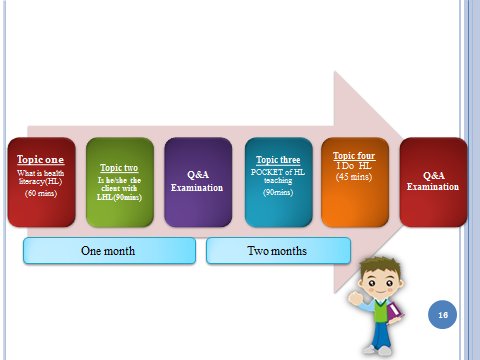
Topic one Topic two


Topic three Topic four


This program has the contributions on the efficacy of use an online platform for on-the-job training with the expectation of lowering the limitations of typical classroom lessons. Though supported by hospitals, there is still room for discussion in terms of the program’s degree of participation and feedback. Also, it was discovered that 3 participants have yet to access the program and only completed the Q&A. Whether this will affect the effectiveness of the intervention awaits further investigation as more diversified platforms with more features will be created for increasing participation.
This project was supported by the Ministry of Science and Technology in Taiwan (NSC100-2511-S-255-001-MY2). The author thanks all participants in the online simulation curriculum and follow-up procedure during the three-month peroid .
 Send Email
Send Email