
|
Authors | Institution |
|
Perez MSD Cassefo G Consolin L Reis M Marques L Guimaraes TVV Chiba T |
Instituto do Cancer do Estado de São Paulo - Palliative Care - São Paulo, Brazil |
 |
|
||||||
| Improving Communication Skills (CS) a medical education experience during a Palliative Care (PC) rotation in an oncological centre in Brazil |
Breaking bad news, discussing goals of care and addressing advance directives are essential components of physician-patient communication (1). However, literature reports significant shortcomings on communication skills training for practising doctors (2). Breaking bad news has been shown to be a stressful experience for doctors even in a simulated encounter, especially for those who were inexperienced (3). The same study correlated poor communication performance to burnout and fatigue (3). Although learning communication skills at the end of life is widely considered important by residents and medical students it is frequently reported as insuficient (1, 4). Fortunately, there is evidence that CS can be taught. Retreats and workshops formats focused on communication training have been shown to improve confidence and performance, but data on a residency format is still limited (5).
During a 1-month Palliative Care (PC) rotation, internal medicine and geriatrics residents undergo training in Communication Skills (CS). It includes role-play sessions and direct observation of family meetings (FM) followed by feedback from faculty.
This is a retrospective study aiming to evaluate this training approach. One hundred residents were invited to answer an anonymous online survey from August 2012 to January 2014, 40 residents answered it. The questions focused on resident’s self-perception of CS.
The demographic characteristics of the 40 participants are described on table 1. Ninety percent of these residents took part on at least 3 FM. According to 71,8%, advance directives were discussed in more than half of these FM. Seventy two percent participated in 3 or more role-play sessions. The role-play sessions focused on breaking bad-news, proposing palliative care, discussing advance directives and dealing with families who don't want the patient be told the truth about his diagnosis and prognosis. Residents considered the feedback provided during these activities (FM and role-play sessions) an outstanding part of their learning process. Eighty five percent said that the feedback provided allowed them to have a different perspective of their own CS.
Table 1) Demografic data, total 40 residents
| Gender | 60% female | 40% male | |
| Age |
from 23 to 33 years |
average age 27 | |
| Ethnic group | 82,5% caucasian | 10% oriental | 7,5% pardo |
| Religion | 51.3% catholic | 18% spiritism | 12,8% atheist |
| Years since graduation in medical school | minimum 2y | maximum 8y | average 4y |
Pardo is a race/skin color category used by the Brazilian Institute of Geography and Statisctics (IBGE) in Brazilian censuses. The term "pardo" is used to refer to mixed race Brazilians, individuals with varied racial ancestries.
After this rotation, the majority of residents reported feeling more confortable to break bad news, propose palliative care, discuss DNR/DNI orders, discuss prognosis and support bereaved family members (table 2). Ninety percent of them related their improvement with this specific trainning and 92.5% said that after the rotation it was easier to deal with emotion brought on by both patient and family.
Table 2) How residents feel towards different aspects of communication after this rotation
| Unconfortable | Partialy Unconfortable | Neutral | Partialy Confortable | Very Confortable | |
| Breaking bad news (diagnosis/prognosis) | 0% | 2.5% | 0% | 40.0% | 57.5% |
| Proposing palliative care | 0% | 5.0% | 0% | 57.5% | 37.5% |
| Discussing suspension of treatment | 0% | 2.5% | 5% | 55.0% | 37.5% |
| Supporting bereaved family | 2,5% | 0% | 5% | 40.0% | 52.5% |
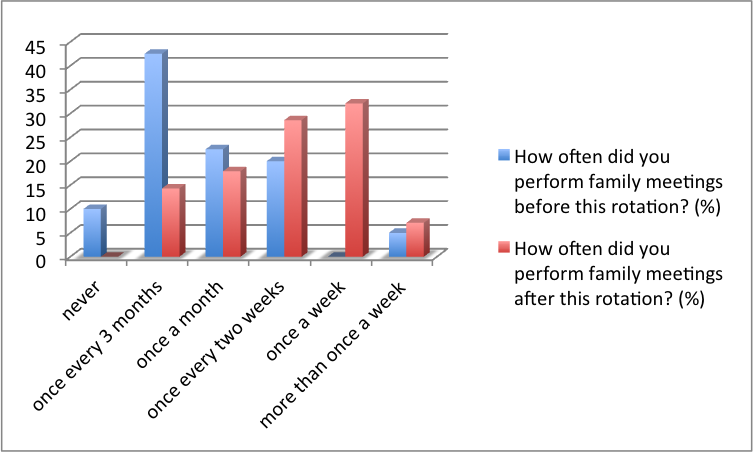
While 52,3% of the residents referred performing less them 1 FM every 3 months before the rotation, after this intervention 60% were conducting FM at least once a month (grafic 1) and 80% reported being able to use these skills in other non-oncological contexts.
Grafic 1) Frequency of family meeting before and after the rotation:
Despite being a retrospective study, analyzing residents self-perceptions without external evaluation of their actual performance, it seems that a specific training intervention focusing CS is likely to improve residents abilities to better establish patient-physician communication.
It is interesting to notice the considerable increase in frequency of family meetings before and after this rotation, which could indicate that residents were able to include this very usefull tool in their own practice. Another interesting point is that although the rotation was in an oncological palliative care service the participants refered that they were able to use the CS acquired in other contexts.
CS improvement could be attained by exposure to practice and constructive feedback.
Palliative care sevices can be an interesting set to develop CS.
1) Furman CD, Head B, Lazor B, Casper B, Ritchie CS. Evaluation of an educational intervention to encourage advance directive discussions between medicine residents and patients. Journal of Palliative Medicine. 2006 Aug;9(4):964–7.
2) Cegala DJ, Lenzmeier Broz S. Physician communication skills training: a review of theoretical backgrounds, objectives and skills. Medical Education. 2002 Nov;36(11):1004–16.
3) Brown R, Dunn S, Byrnes K, Morris R, Heinrich P, Shaw J. Doctors' stress responses and poor communication performance in simulated bad-news consultations. Acad Med. 2009 Nov;84(11):1595–602.
4) Sullivan AM, Lakoma MD, Block SD. The status of medical education in end-of-life care: a national report. J Gen Intern Med. 2003 Sep;18(9):685-95.
5) Szmuilowicz E, el-Jawahri A, Chiappetta L, Kandar M, Block S. Improving residents end-of-life communication skills with a short retreat: a randomized controlled trial. Journal of Palliative Medicine. 2010 Apr; 13(4): 439-52
 Send Email
Send Email
